The study conducted a near atomic resolution analysis of the variant using a cryo-electron microscope

People queue up for their Covid-19 vaccine booster shots at a clinic inside the Metro Toronto Convention Centre, as the latest Omicron variant emerges as a threat, in Toronto, Ontario, Canada. (REUTERS)
Updated on Dec 23, 2021
By Anirudh Bhattacharyya
Canadian researchers on Wednesday revealed, what they say, is the first molecular structural analysis of the Omicron variant of Covid-19 in the country which has shown that it has three to five times more mutations in its spike protein than any previous variant.
A near atomic resolution analysis of the variant using a cryo-electron microscope, “reveals how the heavily mutated variant infects human cells and is highly evasive of immunity,” the Canadian researchers at the University of British Columbia (UBC), which conducted the study, said.
Dr Subramaniam, a professor in the faculty of medicine’s department of biochemistry and molecular biology who led the study, described Omicron having 37 spike protein mutations as “unprecedented”.
“This is important for two reasons. Firstly, because the spike protein is how the virus attaches to and infects human cells. Secondly, because antibodies attach to the spike protein in order to neutralize the virus. Therefore, small mutations on the spike protein have potentially big implications for how the virus is transmitted, how our body fights it off, and the effectiveness of treatments,” he said.
The pre-publication study at bioRxiv noted the Delta variant had seven mutations in the spike protein and had only two in common with Omicron. “Analysis of the sequence of the Omicron genome suggests that it is not derived from any of the currently circulating variants, and may have a different origin,” the Canadian study stated.
“Our experiments confirm what we’re seeing in the real world — that the Omicron spike protein is far better than other variants at evading monoclonal antibodies that are commonly used as treatments, as well as at evading the immunity produced by both vaccines and natural infection,” Dr Subramanian said. It was, however, less evasive of immunity created by vaccines than that produced through natural infection.
“Sera from convalescent patients shows an even greater drop in neutralization potency relative to the Delta variant (8.2x decrease) while the vaccinated group also shows reduction in potency, although to a lesser extent (3.4x decrease),” the study said.
This point was also stressed upon by Dr Subramaniam, as he said, “This suggests that vaccination remains our best defence against the Omicron variant.”
ABOUT THE AUTHOR
Anirudh Bhattacharyya is a Toronto-based commentator on North American issues, and an author. He has also worked as a journalist in New Delhi and New York spanning print, television and digital media. He tweets as @anirudhb
Could Omicron have been predicted? First-of-its-kind technology possibly foresees variants
By Noor Ibrahim Global News
Posted December 24, 2021

What would predicting a variant mean for pandemic preparedness and vaccine manufacturing? Noor Ibrahim talks to a team of researchers that believe their technology can accomplish a first-of-its-kind feat in Canada.
From a fake movie poster allegedly predicting its arrival in the 1960s to a hoax Simpsons episode foreshadowing widespread panic, there’s been no shortage of speculation that the onset of the Omicron COVID-19 variant was foreseen way before its arrival.
But while all of those examples have been downgraded to being just plain misinformation, questions do still remain about whether we could have actually seen Omicron coming.
Health officials have long been warning that the coronavirus, and other viruses, mutates as it replicates and infects new hosts – but could they possibly predict what a variant will look like, and how it will behave, way before the virus even mutates?
READ MORE: COVID-19 mutations make pandemic trajectory unpredictable, experts say
A team of researchers at the University of Waterloo believe they’ve come up with a technology that could come pretty close
“It has been shown by us and other researchers that artificial intelligence and text mining algorithms can be used to model genetic codes and predict virus mutations,” said Mohammad Kohandel, lead of the Mathematical Modelling and Biology Lab at the University of Waterloo, and a pioneer on this project alongside Amir Hossein Darooneh and Michelle Przedborski.
The team believes its technology is the first of its kind in the country.
Their secret? Machine learning and genomes — the building block sequence for the virus.
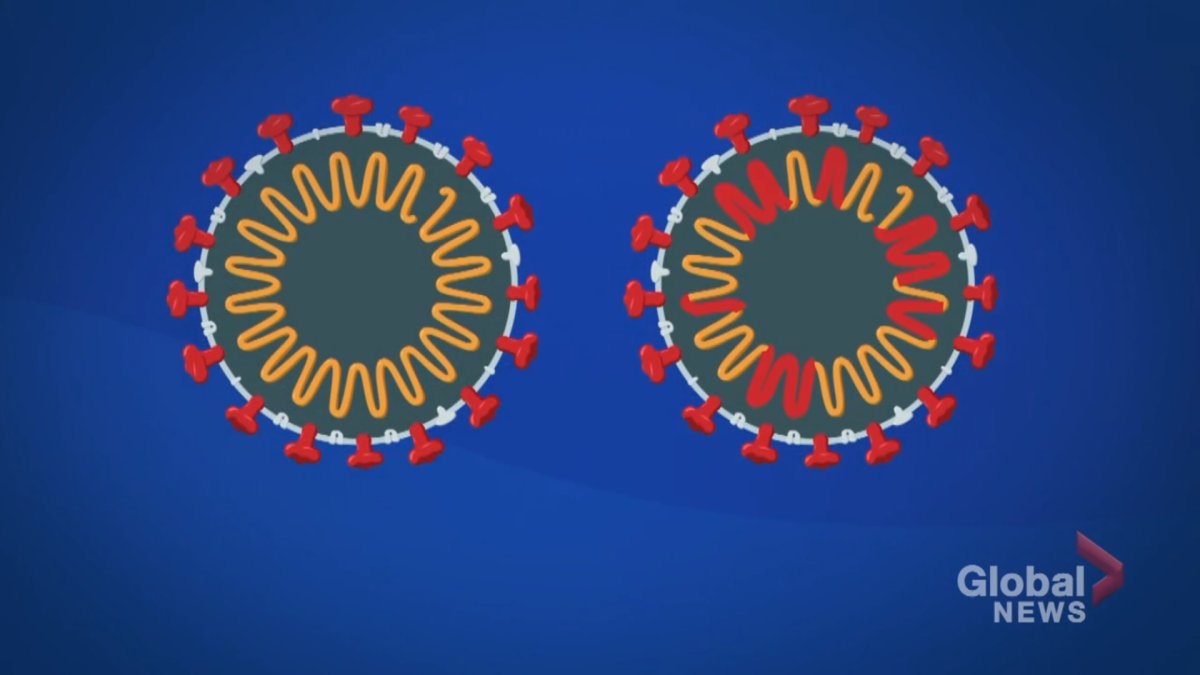
As a virus is copying itself, it will accidentally make “copying errors” or mistakes in the genome sequence, resulting in a mutation. A variant could have one or many mutations within its sequence.
Delta has two mutations in its genome, Kohandel said. Omicron has 50.
By Noor Ibrahim Global News
Posted December 24, 2021

What would predicting a variant mean for pandemic preparedness and vaccine manufacturing? Noor Ibrahim talks to a team of researchers that believe their technology can accomplish a first-of-its-kind feat in Canada.
From a fake movie poster allegedly predicting its arrival in the 1960s to a hoax Simpsons episode foreshadowing widespread panic, there’s been no shortage of speculation that the onset of the Omicron COVID-19 variant was foreseen way before its arrival.

But while all of those examples have been downgraded to being just plain misinformation, questions do still remain about whether we could have actually seen Omicron coming.
Health officials have long been warning that the coronavirus, and other viruses, mutates as it replicates and infects new hosts – but could they possibly predict what a variant will look like, and how it will behave, way before the virus even mutates?
READ MORE: COVID-19 mutations make pandemic trajectory unpredictable, experts say
A team of researchers at the University of Waterloo believe they’ve come up with a technology that could come pretty close
“It has been shown by us and other researchers that artificial intelligence and text mining algorithms can be used to model genetic codes and predict virus mutations,” said Mohammad Kohandel, lead of the Mathematical Modelling and Biology Lab at the University of Waterloo, and a pioneer on this project alongside Amir Hossein Darooneh and Michelle Przedborski.
The team believes its technology is the first of its kind in the country.
Their secret? Machine learning and genomes — the building block sequence for the virus.
As a virus is copying itself, it will accidentally make “copying errors” or mistakes in the genome sequence, resulting in a mutation. A variant could have one or many mutations within its sequence.
Delta has two mutations in its genome, Kohandel said. Omicron has 50.
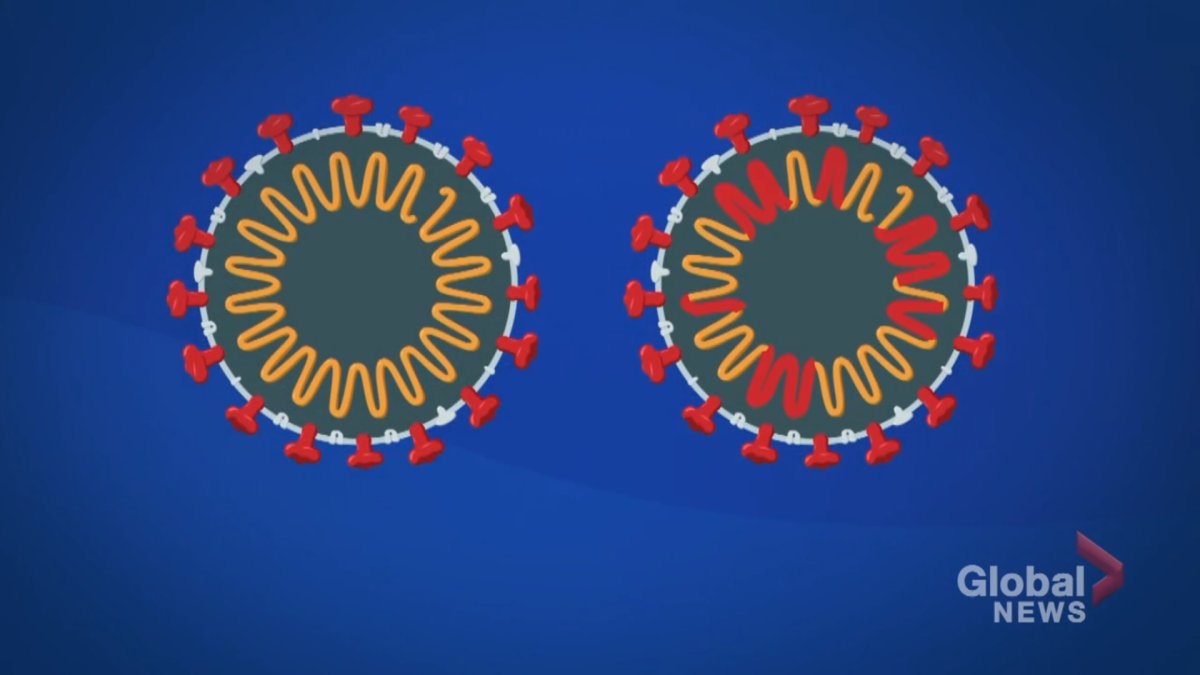
Viruses make ‘copying errors,’ or mutations, when replicating that could make them more or less transmissible. Global GFX for Noor Ibrahim
The parts of the genome that are “conserved,” or stay the same, are the ones targeted by the team’s technology.
Using only the original genome sequence for the COVID-19 virus, artificial intelligence can identify the conserved parts of the genome, and then predict which ones will mutate.
So far, the team has trained the AI to be able to predict — with high accuracy — Alpha, Beta, Delta, Gamma and other variants. It also predicted 19 out of the 50 highly possible mutations for Omicron.
“It is important to highlight that these predictions are not 100, we just gave which ones are more likely to be mutated,” said Kohandel. “It’s very fast and efficient, so we can have the result during hours.”
Headquartered in Ottawa, a team of 57 national researchers are also doing integral work in studying variants.
The Coronavirus Variants Rapid Response Network (CoVaRR-Net), is closely monitoring COVID-19 variants identified across the globe, and is actively trying to pinpoint which ones could become “variants of concern” – meaning variants that have become stronger, more transmissible or more resistant to vaccine through mutations.
“The focus now is mainly on Omicron, but also we’re casting a wider net,” said Jesse Shapiro, Pillar 6 lead in computational biology and modelling and professor at McGill University.
“We’re looking at, for example, if the Delta variant and the Alpha variant infected the same person, could that create a hybrid strain?”
Shapiro says CoVaRR-Net researchers are able to recognize old mutations they’ve seen before, which helps them assess how dangerous a new variant can be, in order to alert health authorities.
“We brief the deputy health minister on at least a weekly basis, if not more. We are in pretty much constant communication with the National Microbiology Laboratory and the Public Health Agency of Canada.”
READ MORE: Omicron’s community transmission could ‘rapidly escalate’ in coming days, Tam warns
Shapiro also says researchers know virus mutations have constraints.
Think of it as swapping words out in a sentence: there’s only so much you can change before the sentence stops making sense. Similarly, a mutation has to make sense within the overall genome sequence – otherwise, it will become gibberish, and the sequence will “break,” said Shapiro.
All this information gives scientists a good idea of what to expect next from a virus — although not 100 per cent.
In any case, knowing which parts of a virus will stay the same is integral in crafting a vaccine that would not be impacted by new variants, both Kohandel and Shapiro stress.
“Canada has an army that is standing and ready to go. This is the sort of analogy that we’d like to have for pandemic preparedness,” Shapiro told Global.
Meanwhile, back at the University of Waterloo, Kohandel and his team are trying to refine their technology further by training the AI’s “neural” network to potentially predict variants in the exact order that they will mutate.
The parts of the genome that are “conserved,” or stay the same, are the ones targeted by the team’s technology.
Using only the original genome sequence for the COVID-19 virus, artificial intelligence can identify the conserved parts of the genome, and then predict which ones will mutate.
So far, the team has trained the AI to be able to predict — with high accuracy — Alpha, Beta, Delta, Gamma and other variants. It also predicted 19 out of the 50 highly possible mutations for Omicron.
“It is important to highlight that these predictions are not 100, we just gave which ones are more likely to be mutated,” said Kohandel. “It’s very fast and efficient, so we can have the result during hours.”
Headquartered in Ottawa, a team of 57 national researchers are also doing integral work in studying variants.
The Coronavirus Variants Rapid Response Network (CoVaRR-Net), is closely monitoring COVID-19 variants identified across the globe, and is actively trying to pinpoint which ones could become “variants of concern” – meaning variants that have become stronger, more transmissible or more resistant to vaccine through mutations.
“The focus now is mainly on Omicron, but also we’re casting a wider net,” said Jesse Shapiro, Pillar 6 lead in computational biology and modelling and professor at McGill University.
“We’re looking at, for example, if the Delta variant and the Alpha variant infected the same person, could that create a hybrid strain?”
Shapiro says CoVaRR-Net researchers are able to recognize old mutations they’ve seen before, which helps them assess how dangerous a new variant can be, in order to alert health authorities.
“We brief the deputy health minister on at least a weekly basis, if not more. We are in pretty much constant communication with the National Microbiology Laboratory and the Public Health Agency of Canada.”
READ MORE: Omicron’s community transmission could ‘rapidly escalate’ in coming days, Tam warns
Shapiro also says researchers know virus mutations have constraints.
Think of it as swapping words out in a sentence: there’s only so much you can change before the sentence stops making sense. Similarly, a mutation has to make sense within the overall genome sequence – otherwise, it will become gibberish, and the sequence will “break,” said Shapiro.
All this information gives scientists a good idea of what to expect next from a virus — although not 100 per cent.
In any case, knowing which parts of a virus will stay the same is integral in crafting a vaccine that would not be impacted by new variants, both Kohandel and Shapiro stress.
“Canada has an army that is standing and ready to go. This is the sort of analogy that we’d like to have for pandemic preparedness,” Shapiro told Global.
Meanwhile, back at the University of Waterloo, Kohandel and his team are trying to refine their technology further by training the AI’s “neural” network to potentially predict variants in the exact order that they will mutate.
Alpha variant evolved to suppress the immune system and Omicron shares a similar mutation: study
Alexandra Mae Jones
To look deeper into how the Alpha variant worked, researchers looked at lab-grown cells infected by this variant to monitor protein levels and how the cells functioned.
They then compared the data to how cells responded to infection with the original strain of COVID-19. The biggest difference was in how the body’s innate immune response reacted — or didn’t. This is the body’s first line of defence, which attempts to keep pathogens from entering. Researchers say Alpha interfered with the rallying cry that usually activates this system.
Inside cells infected with Alpha were an abundance of three viral proteins that are known to help COVID-19 avoid the immune response. One in particular, called Orf9b, achieved this by blocking a protein in our cells that normally switches on the genes that signal our immune system to react.
Researchers said in the study that this type of mutation could have contributed to enhanced transmission of the Alpha variant by suppressing more of that early immune response, which may have allowed for the variant to replicate faster.
These findings show that the spike protein isn’t the only factor researchers should be thinking about when designing treatments to help those infected with COVID-19.
As SARS-CoV-2 uses spike proteins on its surface to attach to receptors in a person’s cells, mutations around spike proteins are often talked about more than other types. With the Delta variant, a more efficient spike protein is thought to help it fuse to our cells better, and all of the current COVID-19 vaccines are targeted to get our cells to produce immune responses against this spike protein.
“The mutations in spike allow the virus to get into cells more effectively,” Devan Krogan, one of the authors of the paper and lead of the University of California San Francisco’s Quantitative Biosciences Institute (QBI) and its Coronavirus Research Group (QCRG), said in a press release.
“But what about after the virus gets into cells? There may be other mutations that allow it to replicate more.”
Although each variant is different, many share similar mutations, with both Delta and Omicron appearing as cousins of the Alpha variant. Delta and Omicron both have similar mutations in the areas that researchers studied of the Alpha variant, which means they could be having similar impacts on the immune system.
“The virus will keep evolving and adapting to the host, and every time it will adapt better and better,” Lorena Zuliani-Alvarez, a co-author and senior scientist at the QBI, said in the release. “That’s why Omicron has 53 mutations.”
The research points out that studying mutations outside of those around the spike protein will give scientists a bigger picture of the virus as it evolves, something that will be crucial in fighting future variants.
“Studying the variants of concern gives us ideas about how SARS-CoV-2 evolves,” Mehdi Bouhaddou, a postdoctoral scholar and co-author, said in the release. “Now we have a sense of the proteins that are mutating most frequently, and the biological consequences of those mutations. I think this helps us prepare for what might come next.”
Alexandra Mae Jones
CTVNews.ca writer
Saturday, December 25, 2021
New research investigating how the very first variant of concern for the novel coronavirus developed has found that the Alpha variant evolved mutations that suppressed specific aspects of the immune system, similar to mutations seen in newer variants such as Omicron.
The Alpha variant first emerged in the U.K. in the fall of 2020, introducing the world to the frightening idea of variants of SARS-CoV-2, the virus that causes COVID-19. Although it has since been outstripped by subsequent variants including Delta and Omicron, studying Alpha’s structure and function helps scientists better understand how virus variants evolve.
Researchers from the U.S. and the U.K. worked together to investigate how Alpha attacked the human body, and found that the mutations that allowed it to thrive go beyond just those centred around the spike protein.
Their research, described in the journal Nature on Thursday, discovered that the Alpha variant upped production of a specific protein that could help it suppress how infected cells signalled the immune system.
Saturday, December 25, 2021
New research investigating how the very first variant of concern for the novel coronavirus developed has found that the Alpha variant evolved mutations that suppressed specific aspects of the immune system, similar to mutations seen in newer variants such as Omicron.
The Alpha variant first emerged in the U.K. in the fall of 2020, introducing the world to the frightening idea of variants of SARS-CoV-2, the virus that causes COVID-19. Although it has since been outstripped by subsequent variants including Delta and Omicron, studying Alpha’s structure and function helps scientists better understand how virus variants evolve.
Researchers from the U.S. and the U.K. worked together to investigate how Alpha attacked the human body, and found that the mutations that allowed it to thrive go beyond just those centred around the spike protein.
Their research, described in the journal Nature on Thursday, discovered that the Alpha variant upped production of a specific protein that could help it suppress how infected cells signalled the immune system.
To look deeper into how the Alpha variant worked, researchers looked at lab-grown cells infected by this variant to monitor protein levels and how the cells functioned.
They then compared the data to how cells responded to infection with the original strain of COVID-19. The biggest difference was in how the body’s innate immune response reacted — or didn’t. This is the body’s first line of defence, which attempts to keep pathogens from entering. Researchers say Alpha interfered with the rallying cry that usually activates this system.
Inside cells infected with Alpha were an abundance of three viral proteins that are known to help COVID-19 avoid the immune response. One in particular, called Orf9b, achieved this by blocking a protein in our cells that normally switches on the genes that signal our immune system to react.
Researchers said in the study that this type of mutation could have contributed to enhanced transmission of the Alpha variant by suppressing more of that early immune response, which may have allowed for the variant to replicate faster.
These findings show that the spike protein isn’t the only factor researchers should be thinking about when designing treatments to help those infected with COVID-19.
As SARS-CoV-2 uses spike proteins on its surface to attach to receptors in a person’s cells, mutations around spike proteins are often talked about more than other types. With the Delta variant, a more efficient spike protein is thought to help it fuse to our cells better, and all of the current COVID-19 vaccines are targeted to get our cells to produce immune responses against this spike protein.
“The mutations in spike allow the virus to get into cells more effectively,” Devan Krogan, one of the authors of the paper and lead of the University of California San Francisco’s Quantitative Biosciences Institute (QBI) and its Coronavirus Research Group (QCRG), said in a press release.
“But what about after the virus gets into cells? There may be other mutations that allow it to replicate more.”
Although each variant is different, many share similar mutations, with both Delta and Omicron appearing as cousins of the Alpha variant. Delta and Omicron both have similar mutations in the areas that researchers studied of the Alpha variant, which means they could be having similar impacts on the immune system.
“The virus will keep evolving and adapting to the host, and every time it will adapt better and better,” Lorena Zuliani-Alvarez, a co-author and senior scientist at the QBI, said in the release. “That’s why Omicron has 53 mutations.”
The research points out that studying mutations outside of those around the spike protein will give scientists a bigger picture of the virus as it evolves, something that will be crucial in fighting future variants.
“Studying the variants of concern gives us ideas about how SARS-CoV-2 evolves,” Mehdi Bouhaddou, a postdoctoral scholar and co-author, said in the release. “Now we have a sense of the proteins that are mutating most frequently, and the biological consequences of those mutations. I think this helps us prepare for what might come next.”
No comments:
Post a Comment