HUMAN GUINEA PIG
Why pig-to-human heart transplant is for now only a last resortAnalysis: As doctors monitor world’s first human recipient of pig heart, safety and ethical concerns remain

Surgeons at the University of Maryland Medical Center transplanted a heart from a pig into 57-year-old David Bennett.
Photograph: University of Maryland School of Medicine (UMSOM)/EPA
Ian Sample
Ian Sample
Science editor
THE GUARDIAN
Tue 11 Jan 2022
The world’s first transplant of a genetically altered pig heart into an ailing human is a landmark for medical science, but the operation, and the approach more broadly, raise substantial safety and ethical concerns.
Surgeons at the University of Maryland Medical Center spent eight hours on Friday evening transplanting the heart from the pig into 57-year-old David Bennett, who had been in hospital for more than a month with terminal heart failure.
It was an exceptional procedure. Doctors considered Bennett to be facing near-certain death and deemed him too ill to qualify for a routine human heart transplant. As a last resort, the medical team sought emergency authorisation from the Food and Drug Administration (FDA) to transplant a heart from a genetically altered pig.
The heart came from a the pig created by Revivicor, a spin-out from PPL Therapeutics, the UK company that created Dolly the Sheep in 1996. Now under US ownership, Revivicor’s pigs are engineered to avoid immune rejection. Among the genetic alterations made are tweaks that remove a sugar molecule from the tissues that provokes organ rejection. The FDA approved the operation, along with the team’s proposal to use an experimental drug to prevent Bennett’s body from rejecting the organ.
THE GUARDIAN
Tue 11 Jan 2022
The world’s first transplant of a genetically altered pig heart into an ailing human is a landmark for medical science, but the operation, and the approach more broadly, raise substantial safety and ethical concerns.
Surgeons at the University of Maryland Medical Center spent eight hours on Friday evening transplanting the heart from the pig into 57-year-old David Bennett, who had been in hospital for more than a month with terminal heart failure.
It was an exceptional procedure. Doctors considered Bennett to be facing near-certain death and deemed him too ill to qualify for a routine human heart transplant. As a last resort, the medical team sought emergency authorisation from the Food and Drug Administration (FDA) to transplant a heart from a genetically altered pig.
The heart came from a the pig created by Revivicor, a spin-out from PPL Therapeutics, the UK company that created Dolly the Sheep in 1996. Now under US ownership, Revivicor’s pigs are engineered to avoid immune rejection. Among the genetic alterations made are tweaks that remove a sugar molecule from the tissues that provokes organ rejection. The FDA approved the operation, along with the team’s proposal to use an experimental drug to prevent Bennett’s body from rejecting the organ.
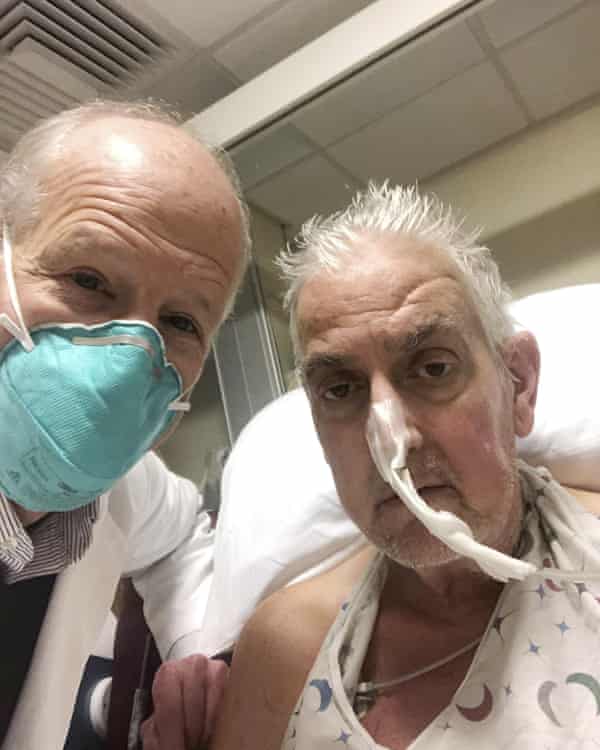
Dr Bartley Griffith with David Bennett , the world’s first human recipient of a pig heart.
Photograph: Bartley Griffith/AP
On Monday, doctors at the hospital said Bennett was awake and breathing on his own, but it was too soon to call the operation a success. Doctors are waiting to see how Bennett fares in the coming days, weeks and hopefully months.
The prospect of harvesting organs from animals to save human lives has a long and chequered history. Advocates see the approach as a way to slash waiting lists for desperately ill patients, while animal rights activists see it as dangerous and ethically abhorrent. In the 1960s, US doctors transplanted chimp kidneys into more than a dozen patients, all but one of whom died within weeks. In the 1980s, a premature baby in California received a baboon heart but died three weeks later.

Maryland doctors transplant pig’s heart into human patient in medical first
The main risk is immune rejection: even with organs from human donors, recipients need constant immunosuppression to prevent their bodies from attacking the transplants. While Revivicor’s pig heart is designed to be less prone to immune rejection than standard animal organs, it is unclear how well it will be tolerated by the body. Because the organ comes from another species, Bennett will need more potent immunosuppression than usual, which comes with its own medical risks.
Recent work on such donor animals has focused on pigs because, although they have different immune systems to humans, the animals’ organs are very similar. While much of the effort has been directed at making pig organs invisible to the human immune system, it is far from the only challenge. In the 1990s, scientists all but abandoned their work on donor pigs when they realised that retroviruses lurking in the animals’ DNA could potentially infect human cells. That raised the worrying prospect of transplanted organs spreading infection to the vulnerable patients who received them.
Research has been under way to overcome the problem, by taking genome editing to another level. After tweaking pig DNA to remove molecules that trigger immune rejection, scientists have made precision alterations that remove dozens of retroviruses from pig tissues in the hope the organs will be safer when they are eventually transplanted.
How well animal organs work will be for clinical trials to decide, rather than one-off operations. Many biotech companies are moving cautiously, setting up trials to check whether the organs are safe and effective, first in other animals and then in humans. For those with failing organs, the hope for now remains with the generosity of human donors.
On Monday, doctors at the hospital said Bennett was awake and breathing on his own, but it was too soon to call the operation a success. Doctors are waiting to see how Bennett fares in the coming days, weeks and hopefully months.
The prospect of harvesting organs from animals to save human lives has a long and chequered history. Advocates see the approach as a way to slash waiting lists for desperately ill patients, while animal rights activists see it as dangerous and ethically abhorrent. In the 1960s, US doctors transplanted chimp kidneys into more than a dozen patients, all but one of whom died within weeks. In the 1980s, a premature baby in California received a baboon heart but died three weeks later.

Maryland doctors transplant pig’s heart into human patient in medical first
The main risk is immune rejection: even with organs from human donors, recipients need constant immunosuppression to prevent their bodies from attacking the transplants. While Revivicor’s pig heart is designed to be less prone to immune rejection than standard animal organs, it is unclear how well it will be tolerated by the body. Because the organ comes from another species, Bennett will need more potent immunosuppression than usual, which comes with its own medical risks.
Recent work on such donor animals has focused on pigs because, although they have different immune systems to humans, the animals’ organs are very similar. While much of the effort has been directed at making pig organs invisible to the human immune system, it is far from the only challenge. In the 1990s, scientists all but abandoned their work on donor pigs when they realised that retroviruses lurking in the animals’ DNA could potentially infect human cells. That raised the worrying prospect of transplanted organs spreading infection to the vulnerable patients who received them.
Research has been under way to overcome the problem, by taking genome editing to another level. After tweaking pig DNA to remove molecules that trigger immune rejection, scientists have made precision alterations that remove dozens of retroviruses from pig tissues in the hope the organs will be safer when they are eventually transplanted.
How well animal organs work will be for clinical trials to decide, rather than one-off operations. Many biotech companies are moving cautiously, setting up trials to check whether the organs are safe and effective, first in other animals and then in humans. For those with failing organs, the hope for now remains with the generosity of human donors.
No comments:
Post a Comment