AUSTRALIA
AUSTERITY CREATED CRISIS
NSW inquiry into ambulance ramping told patients 'dying unnecessarily'SAME AS IN CANADA
The inquiry has been told ambulance ramping is not a rare occurrence in NSW
More testimonies are expected over the two days of the inquiry
The upper house inquiry is examining why ambulances are becoming stuck at hospitals, unable to offload their patients, and how emergency departments are coping.
Western Sydney-based emergency medicine staff specialist, James Tadros, told the inquiry that doctors felt they were "failing the needs of patients on a daily basis".
"We work in an environment that we don't see as conducive to good medical care," he said.
"These people we serve bear the brunt of our failing system."
The inquiry heard that most hospitals, particularly in Western Sydney, are operating at 100 per cent capacity.

abc.net.au
ABC-TODAY

ABC-TODAY
The NSW inquiry has heard that hospitals in Western Sydney are operating at 100 per cent.
(AAP: Bianca De Marchi)
Patients are "dying unnecessarily" while waiting in hospital emergency departments in what one doctor has called "third world" conditions, a NSW parliamentary inquiry has heard.
Key points:
Key points:
Doctors have told the NSW inquiry that hospitals in Western Sydney are running at 100 per cent capacity
The inquiry has been told ambulance ramping is not a rare occurrence in NSW
More testimonies are expected over the two days of the inquiry
The upper house inquiry is examining why ambulances are becoming stuck at hospitals, unable to offload their patients, and how emergency departments are coping.
Western Sydney-based emergency medicine staff specialist, James Tadros, told the inquiry that doctors felt they were "failing the needs of patients on a daily basis".
"We work in an environment that we don't see as conducive to good medical care," he said.
"These people we serve bear the brunt of our failing system."
The inquiry heard that most hospitals, particularly in Western Sydney, are operating at 100 per cent capacity.
James Tadros has told the inquiry doctors felt they were failing patients.
(ABC News)
Dr Tadros recalled an incident in which an 88-year-old patient with kidney failure was waiting to be seen for several hours.
"I found her [in the waiting room] laying down across three chairs and some bystanders were helping her daughter to slowly move her around because she was so weak," he said.
"This is basically third world."
When asked by Labor's Rose Jackson if patients waiting in emergency departments were "dying unnecessarily" because of a lack of adequate care, Dr Tadros replied, "Yes...you do see patients who deteriorate while waiting to be seen."
The inquiry heard the increased pressure on frontline staff was leading to high rates of burnout, with many opting to leave the workforce.
"The frontline staff have become completely numb to it," Setthy Ung from the South Western Sydney Local Health District said.
"They've learnt to adapt, to live on the knife's edge."
Dr Tadros recalled an incident in which an 88-year-old patient with kidney failure was waiting to be seen for several hours.
"I found her [in the waiting room] laying down across three chairs and some bystanders were helping her daughter to slowly move her around because she was so weak," he said.
"This is basically third world."
When asked by Labor's Rose Jackson if patients waiting in emergency departments were "dying unnecessarily" because of a lack of adequate care, Dr Tadros replied, "Yes...you do see patients who deteriorate while waiting to be seen."
The inquiry heard the increased pressure on frontline staff was leading to high rates of burnout, with many opting to leave the workforce.
"The frontline staff have become completely numb to it," Setthy Ung from the South Western Sydney Local Health District said.
"They've learnt to adapt, to live on the knife's edge."
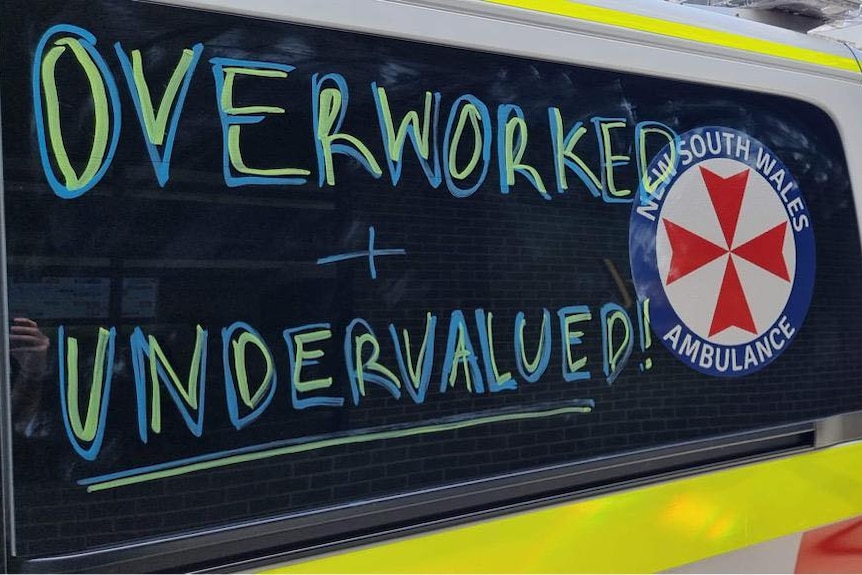
Paramedics say they have been calling for more staff and funding for the past decade.(Supplied: Australian Paramedics' Association NSW)
Earlier, the paramedics union accused the NSW Health Minister Brad Hazzard of being "out of touch", after he suggested ambulance ramping was "rare" in the state.
Mr Hazzard told a budget estimates hearing in March that ambulance ramping which "causes major grief in other states" is "actually very rare in New South Wales".
Vice President of the Australian Paramedics Association NSW, Scott Beaton, told the inquiry the comments were inaccurate.
"I laughed to be perfectly honest," Mr Beaton said.
"It was just a statement to show the Minister [Hazzard] or his advisors are out of touch with what's happening in the hospitals."
Clare Skinner, president of the Australasian College of Emergency Medicine, acknowledged that while NSW "does well compared to other states", ambulance ramping was "not rare, it's common".
She said overcrowding in emergency departments and "access block" — where patients who have been treated in an emergency department are unable to access hospital beds in a timely manner — was now the "new normal".
"It has now become a permanent state of being in emergency departments in NSW," Dr Skinner said.
What's causing long hospital wait times?
Adding more beds won't fix emergency department pressures. Neither will one-size-fits-all processes. But improving patient flow and addressing staff shortages might.
Earlier, the paramedics union accused the NSW Health Minister Brad Hazzard of being "out of touch", after he suggested ambulance ramping was "rare" in the state.
Mr Hazzard told a budget estimates hearing in March that ambulance ramping which "causes major grief in other states" is "actually very rare in New South Wales".
Vice President of the Australian Paramedics Association NSW, Scott Beaton, told the inquiry the comments were inaccurate.
"I laughed to be perfectly honest," Mr Beaton said.
"It was just a statement to show the Minister [Hazzard] or his advisors are out of touch with what's happening in the hospitals."
Clare Skinner, president of the Australasian College of Emergency Medicine, acknowledged that while NSW "does well compared to other states", ambulance ramping was "not rare, it's common".
She said overcrowding in emergency departments and "access block" — where patients who have been treated in an emergency department are unable to access hospital beds in a timely manner — was now the "new normal".
"It has now become a permanent state of being in emergency departments in NSW," Dr Skinner said.
What's causing long hospital wait times?
Adding more beds won't fix emergency department pressures. Neither will one-size-fits-all processes. But improving patient flow and addressing staff shortages might.
Read more
Dr Skinner noted that the issue was "not a COVID phenomenon" and was present for decades before the pandemic.
"It's fair to say that COVID was the straw that broke the camel's back," she said.
"This is a global phenomenon which been growing for decades due to underinvestment, under-resourcing and poor coordination of community-based care."
She suggested that solutions focus on improving capacity at hospital wards and boosting investment in community-based care to allow for earlier discharge into primary care.
Dr Skinner said there was a "crisis" in emergency department staffing.
"I often wonder what it takes for our emergency department workforce to break," she said.
"We keep pulling that extra bit out of the tank ... but the kettle feels dry at the moment."
The inquiry will run for two days.
Dr Skinner noted that the issue was "not a COVID phenomenon" and was present for decades before the pandemic.
"It's fair to say that COVID was the straw that broke the camel's back," she said.
"This is a global phenomenon which been growing for decades due to underinvestment, under-resourcing and poor coordination of community-based care."
She suggested that solutions focus on improving capacity at hospital wards and boosting investment in community-based care to allow for earlier discharge into primary care.
Dr Skinner said there was a "crisis" in emergency department staffing.
"I often wonder what it takes for our emergency department workforce to break," she said.
"We keep pulling that extra bit out of the tank ... but the kettle feels dry at the moment."
The inquiry will run for two days.
No comments:
Post a Comment