Cara McGoogan
Sun, 17 September 2023

tainted blood
Kevin Slater had been in and out of hospital with unexplained symptoms including rapid weight loss and acid reflux for three months by March 1983, when his doctor started to suspect he could be suffering from a new illness called acquired immunodeficiency disorder, or Aids, which had emerged in America two years earlier and was predominantly affecting gay men.
A 20-year-old precision-tool engineer from Cwmbran, in South Wales, Kevin had never been to the United States, he wasn’t gay and he didn’t use intravenous drugs.
If he had Aids, there was only one way he could have contracted it – from Factor VIII, a “miracle” treatment for haemophilia made from human plasma.
Prof Arthur Bloom, Kevin’s doctor at the University Hospital of Wales in Cardiff, was Britain’s leading haematologist. Not wanting to cause panic about Factor VIII, despite his concern that it could be contaminated, Bloom hedged Kevin’s diagnosis and downplayed the risk of Aids for people with haemophilia for months.

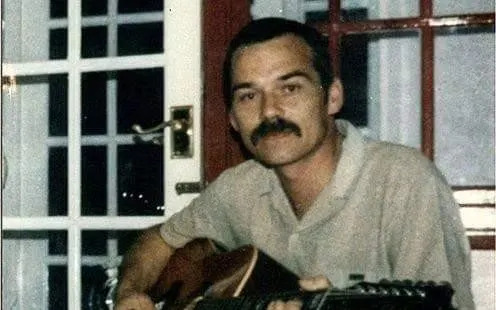
Kevin Slater, as well as his brother Paul, was treated with contaminated Factor VIII
Kevin rapidly became ill, and in May 1983, he was the first British person with haemophilia to be diagnosed with Aids. Four months later, an anonymous man in Bristol died from an Aids-related illness after treatment with Factor VIII. Kevin and the man in Bristol were the first official casualties of what would become known as the infected blood scandal, described as “the worst treatment disaster in the history of the National Health Service”, in which an estimated 2,900 people have died after contracting HIV and hepatitis C from contaminated blood products or transfusions.
Forty years on, the Infected Blood Inquiry, set up by Theresa May in 2017, is due to report this autumn on how so many people were infected with HIV and hepatitis C, and the ensuing cover-up. The results could lead to compensation amounting to billions of pounds.
I have spent two years speaking to survivors, lawyers, doctors and politicians for my book The Poison Line, which investigates how Bloom concealed evidence, the Department of Health endangered patients with its sluggish response to the Aids crisis and pharmaceutical companies put profits above lives.
Kevin was an ebullient young man who liked to drink the occasional half a pint in the evening. By March 1983, he had become unnaturally tired, developed severe reflux oesophagitis and oral thrush, and lost a stone in weight. On March 17, his test results came back from the laboratory with a worrying possibility: “?Aids”.
Since birth, Kevin had been treated for haemophilia A, first with cryoprecipitate then with Factor VIII. In the 1980s, Britain imported half of its Factor VIII from the US, where pharmaceutical companies paid for plasma from prisons, Skid Row and clinics for sexually transmitted diseases, before pooling tens of thousands of donations together. If one donor had an infectious virus, that batch of Factor VIII was contaminated.
Doctors and politicians had known about the risks of imported commercial Factor VIII since the 1970s, but still the British government had continued to rely on it.
In July 1982, after three haemophiliacs in the US contracted Pneumocystis-carinii pneumonia (PCP), a rare and often fatal fungal infection in the lungs, rumours began circulating in medical circles that Factor VIII could be connected to an immune-related syndrome that was affecting gay men
By the following year, researchers were honing in on the theory that Aids was transmitted through an infectious agent in blood and could therefore have made it into Factor VIII. On March 4, 1983, the US Centers for Disease Control (CDC) named people with haemophilia as one of the four most at-risk groups in its first Aids trends report. “Blood products or blood appear responsible for Aids among haemophilia patients who require clotting factor,” said the CDC.
Seeking advice for Britain, Bloom wrote to Bruce Evatt, director of haematology at the CDC, who said there had been 13 cases of Aids confirmed in Americans with haemophilia, with another five “highly suspected”. “I suspect it is a matter of time before you begin to see cases in the United Kingdom,” wrote Evatt.
But when Kevin showed symptoms of Aids a couple of weeks later, Bloom prevaricated and told the Haemophilia Society there weren’t “any definite cases in British haemophiliacs”.
On May 1, The Mail on Sunday ran a front page story saying that NHS hospitals were using “killer blood” imported from America. The article was met with a backlash from influential doctors. Bloom wrote to the Haemophilia Society and said: “We are unaware of any proven case in our own haemophiliac population… Whilst it would be wrong to be complacent, it would be equally counterproductive to alter our treatment programmes radically.” Peter Jones, director of the haemophilia centre in Newcastle, complained to the Press Council, saying the piece by Sue Douglas was “neither objective nor accurate”. The Press Council upheld the complaint and told The Mail on Sunday to sanction Douglas. “It was about shooting the messenger,” says Douglas.
If her reporting had been heeded, lives could have been saved. As recently as this year a man contacted her to say he believed she had saved his life: after reading her article, his parents had demanded that his doctor stop treating him with Factor VIII.
Throughout the summer of 1983, evidence mounted that Aids was transmitted through an infectious agent in blood, and could therefore be in Factor VIII. In an internal document kept from the public, the Department of Health accepted that “the assumption is that such transmission is possible”. The Council of Europe said doctors and patients should be warned about the “health hazards” of Factor VIII and advised countries to stop importing the commercial version made from large pools of donations.
But in June 1983, two months after Kevin was officially recorded as having Aids, Bloom still equivocated. Kevin had a vomiting bug and suspected PCP, but Bloom said his diagnosis was only “possible” and “cannot be described as a definite case”.
During my research for The Poison Line I uncovered new evidence that Bloom in fact suspected at least six other patients could have contracted Aids from being treated with the same batch of Factor VIII he believed had infected Kevin. He wrote to their doctors saying: “Although our patient may not be suffering from Aids, I nevertheless thought you should know.” As the leading adviser on haemophilia care, Bloom’s refusal to admit the dangers of Factor VIII had fatal consequences. The Government was consequently slow to respond to the risk of Aids in blood products, never banning risky American imports, and leaving patients in the dark. Dissenting voices were ignored.

Demonstrators during July as Rishi Sunak was questioned by the Infected Blood Inquiry in London - Getty
By September 1983, when the first haemophiliac in Bristol died from an Aids-related illness, the Department of Health had adopted Bloom’s evasive language, saying “there is no underlying conclusive evidence” that Aids could be transmitted through blood products.
As Kevin’s health deteriorated he stopped working and seeing his friends. After people in his neighbourhood discovered he had Aids, they began crossing the street to avoid him. The stigma only worsened when his older brother, Paul, tested positive for HIV, having also been treated with Factor VIII. The postman started leaving their mail at the end of the driveway.
Within a month of his diagnosis, Paul gave up his job in electronics. “He didn’t want to go on,” Lynda Maule, his partner of five years, said in inquiry evidence.
Soon after, Paul split up with Maule, who was the mother of his young daughter, and returned to his parents in Cwmbran. His mother, who worked in a school, had to give up her job in order to look after her two sons.
In mid-June 1985, Kevin was admitted to hospital with pneumonia and put on an isolation ward. Staff were reluctant to enter his room, so his family brought him food. They had to feed him themselves, because he was “as weak as a kitten”.
Kevin died a week later on June 23, 1985, aged 22. The funeral director was scared to enter his room to collect the body because of the fear of transmission. When he heard Kevin had died, Paul wanted to run away, but he could barely walk, weighing only 4st 7lb. He tried to conceal how shrunken he had become by wrapping bandages around his legs and layering up with jumpers. But on Aug 4, 1991, Paul too died from Aids, aged 31.
“Paul, Kevin and their parents trusted the medical staff to give them safe medication,” said Maule. “Knowing that such young lives could be taken because of somebody else’s mistake was very hard for everyone.”
In another particularly devastating case, five relatives from the Farrugia family, from Dagenham, east London, contracted viruses from Factor VIII, four of whom died. Barry Farrugia was the first of the family to contract HIV.
A fitter for the North Thames gas board, and a mild haemophiliac, Barry was treated by Bloom after suffering a bleed on his elbow whilst on holiday in Wales.
Documents unearthed by his son Tony, and shared for the first time, reveal that in June 1983 Bloom, who died in 1992, wrote a letter to Barry’s doctor in London saying he had been “given a suspect batch of Factor VIII in 1980”.
“I can only come to the assumption that Bloom knew this stuff was filthy,” says Tony. “He certainly knew there was hepatitis in it.”
Barry died in September 1986, aged 37, leaving a wife and five sons. His younger brother also contracted HIV and died in 2002, while his third brother died from hepatitis C complications in 2012.
In the wake of Barry’s infection and death, the Farrugia family fell apart. Tony went to live with his estranged birth mother, but soon ended up in care. His twin brother David was kicked out by their stepmother after Barry’s death and moved into a separate home 100 miles away. They were kept apart until Tony was 18. “The contaminated blood scandal has destroyed my entire family,” says Tony.
Barry Farugia, a haemophiliac, who was treated by Bloom
About 1,250 people with haemophilia tested positive for HIV at hospitals across the UK. Those where doctors used more imported American Factor VIII had a higher incidence of infections.
From 1985 to 2017, what was a treatment disaster became a national scandal, as the British establishment failed to own up to its mistakes – and actively covered up what had happened.
“There is evidence of the cover-up going right to the top,” says Andy Burnham, the former health secretary and the current Mayor of Greater Manchester, who gave highly critical evidence to the inquiry.
The Department of Health shredded documents from the 1970s and 80s which outlined how dangerous Factor VIII was and what doctors had known. Through successive governments, the Department of Health denied that there had been any wrongdoing, and refused to hold a public inquiry. Meanwhile hospitals sporadically disposed of medical records.
Burnham is clear the Government needs to own up to its mistakes. “If you don’t confront people with what you believe to be the truth, no matter how hard it is, then how does the system learn?” he says.
Some survivors and bereaved relatives want to see prosecutions, others are looking for an official apology. All want proper compensation.
“A lot of the blame is going to be on the dead people, like Bloom,” says Tony. “And it’s difficult to prosecute dead people. What I would like desperately is for the Government to actually hold their hands up and say properly, ‘We’re sorry’. And to financially look after these victims for the rest of their lives.” HIV and hepatitis C require complex care, especially for those who are ageing.
To this day, no one has been held accountable for the thousands of infections and deaths in the UK. In France, two leading haemophilia doctors were imprisoned for their role in treating patients with infected blood products, while a further two were given suspended sentences. Laurent Fabius, the prime minister at the time, was found guilty of manslaughter but received no sentence. Many countries held investigations and paid compensation in the 1990s. But in the UK, the wait continues.

Former French prime minister Laurent Fabius - AFP
Meanwhile, Bloom’s legacy remains fraught. “Arthur Bloom was given a hard rap,” says Edward Tuddenham, emeritus professor at University College London, who was mentored by Bloom. “He was in a very invidious and difficult position.”
Prof Liakat Parapia believes that Bloom, who he trained with, wanted to prevent patients from panicking so they would continue to accept Factor VIII treatment. “But it was wrong,” says Parapia. “You have to be honest and truthful. And you have to give the right advice. Prof Bloom has been disgraced.”
The University Hospital of Wales recently removed Bloom’s name and bust from the haemophilia centre after a campaign by bereaved families.
But Parapia lays the greatest portion of blame with the pharmaceutical companies who took inordinate risks, making billions of dollars in the process. “It was almost like a conspiracy,” he says. “We all fell for the marketing because we needed the support and scientific information they were giving. The pharma companies were brainwashing us.”
In Japan and Germany, the pharma companies who made Factor VIII – Baxter, Bayer, Armour, Alpha and Behringwerke, among others – were forced to contribute around half of the funds for the compensation pot.
While the 2,007 core participants of the Infected Blood Inquiry, who include survivors and bereaved family members, await the final report, chairman Sir Brian Langstaff has recommended the Government set up a compensation scheme without delay. “My conclusion is that wrongs were done at individual, collective and systemic levels,” he said in an interim report in April.
Last year, the Government spent £450 million on interim payments of £100,000 for those who were infected with HIV and hepatitis C, but it has ignored Sir Brian’s call to extend those payments to bereaved family members, including parents who lost children and those who were orphaned.
In July, Sir Brian took the unprecedented step of reopening the inquiry to grill Prime Minister Rishi Sunak and other ministers about why they had ignored his recommendation for compensation.
Once more the Government is silent in its response to Sir Brian and survivors fear they will be let down. “This September dad will have been dead longer than he lived,” says Tony. “I hope he gets justice, but I’m not holding out much hope.”
No matter what the outcome, Tony is unsure he will be able to move on. “I don’t know whether we’ll ever get peace from this,” he says, “because it’s still going on – people are still dying. It’s a constant reminder.”
Listen to Bed of Lies, a six-part Telegraph podcast laying bare one of the biggest medical disasters in history, on Apple Podcasts, Spotify or your preferred podcast app
No comments:
Post a Comment