Indoor Air Quality Matters: COVID, Climate Change, and More
Indoor air quality has emerged as a critical public health concern, gaining traction amidst growing recognition of its significance in spreading COVID-19 and many other diseases. Though progress has been slow, several recent developments suggest palpable momentum toward addressing indoor air quality. Late last month, Science published an article by over 40 experts extolling the importance of indoor air quality and urging policymakers worldwide to mandate indoor air quality standards in public buildings. Around the same time, the World Health Organization (WHO) took a meaningful step toward acknowledging the airborne spread of COVID-19 by unveiling its new Airborne Risk Indoor Assessment (ARIA) tool. The WHO also released a report last week that revises and expands the organization’s position on the mechanics of disease transmission. The report recognizes that many diseases “travel through the air,” though it stops short of endorsing concrete safety protocols. In the US, the Advanced Research Projects Agency for Health (ARPA-H) announced a new program to create a scalable platform to monitor and improve indoor air quality in the US. Much work remains to leverage these initiatives fully, but they represent welcome steps in the right direction.
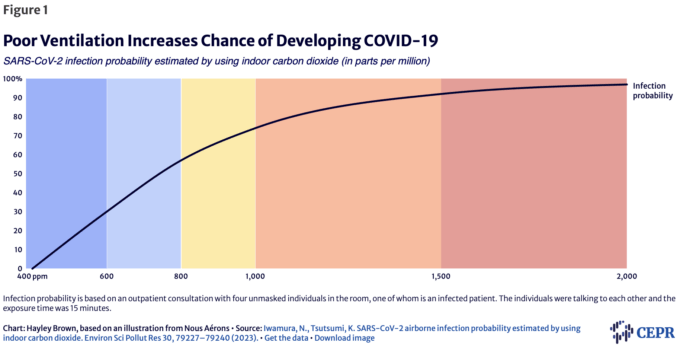
Paralleling the historical significance of water sanitation, indoor air quality is swiftly becoming recognized as a cornerstone public health and workplace safety concern. While the airborne spread of COVID-19 may have thrust indoor air quality into the spotlight, improved indoor air quality can also reduce the spread of other airborne diseases, such as influenza and respiratory syncytial virus (RSV). Upgraded indoor air quality can also cut down on indoor pollution and allergen exposure. Carbon dioxide builds up in crowded, poorly ventilated spaces as people exhale. In the absence of filters or personal protective equipment (PPE) like respirators, this ultimately means that people are more likely to be breathing in each other’s exhalations, alongside whatever other air pollutants may exist in the space. Poor ventilation, as measured by carbon dioxide concentration, is associated with increased spread of diseases such as COVID-19 (Figure 1). Poor indoor air quality indicated by elevated carbon dioxide levels has been linked to reduced productivity and impaired cognition. And while PPE is helpful, safety measures that rely entirely on individual compliance are prone to failure. This is why PPE is at the bottom of the Occupational Health and Safety Administration (OSHA)’s hierarchy of controls for workplace safety. While better indoor air quality would not eliminate every instance of exposure or disease, it would go a long way toward curbing these threats to public health.
Figure 1
Indoor air quality is also a disability rights issue. While everyone is vulnerable to illness and capable of developing long-term sequelae from viruses like SARS-CoV-2 (which causes COVID-19 and Long COVID), those with compromised immune systems and other vulnerabilities may be especially at risk of dire complications from infection. Similarly, while breathing in polluted air isn’t good for anyone’s health, those with asthma and allergies are more likely to suffer from poor indoor air quality. Good indoor air quality is a clear example of universal design; while everyone will benefit, the difference is especially significant for vulnerable and disabled people who might otherwise be unable to make use of the space at all.
Investing in indoor air quality is not only imperative for public health, it is also a sound economic decision. In addition to improving productivity and cognitive performance, ventilation upgrades and high-efficiency particulate air filters (HEPA) appear to cut sick days. Researchers in Australia determined that even before the pandemic, poor indoor air quality cost the country more than $12 billion a year due to ill health and lost productivity, which has undoubtedly increased with the addition of COVID-19. Harvard Professor Joseph Allen estimates that for every $40 per worker per year invested in improved ventilation, employers stand to recoup between $6,000 and $7,000 per worker per year in increased productivity. Not only does the cost-benefit evaluation favor investing in indoor air quality, the campaign for cleaner indoor air has the potential to create good-paying jobs and foster technological innovation.
Indoor air quality also matters for resilience and adaptation to climate change. Because of climate change, communities across the US must now contend with the very real threat of wildfire smoke. Breathing in this smoke is not good for anyone’s health, and with the threat continuing to escalate, now is the time to invest in resilient infrastructure that allows people to breathe clean air indoors despite smoky conditions outside.
Both climate change and the COVID-19 pandemic have had unevenly distributed consequences, with marginalized groups bearing the brunt of both. Poor indoor air quality disproportionately harms marginalized communities, exacerbating existing disparities in health and economic outcomes and lowering resilience to climate change. The consequences of inadequate indoor air quality further entrench inequities and may necessitate targeted interventions to mitigate their impact. It is essential that future investments in indoor air quality are not distributed in a way that leaves marginalized people behind.
All of this makes a compelling case for urgent, robust, and equitable policy action to monitor and improve indoor air quality. Meaningful progress will require ample investment in ventilation and air filtration systems, and may involve both retrofitting existing structures and integrating indoor air quality considerations into new developments. Several professional organizations have already released detailed guidance, including the Ontario Society of Professional Engineers (OSPE) and the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). Transparency and monitoring will also be essential to ensure compliance and to continually assess various interventions. In the US, regulatory bodies, including but not limited to the Environmental Protection Agency (EPA) and the Occupational Safety and Health Administration (OSHA), must be empowered to develop and meaningfully enforce indoor air quality standards. US policymakers can draw some inspiration from international models. Belgium passed legislation requiring carbon dioxide monitors in public spaces and setting targets for acceptable levels. Ireland’s Health and Safety Authority has also promulgated rules requiring employers to carry out workplace indoor air quality risk assessments and to follow guidelines for improvement if those assessments reveal problems.
In the history of epidemiology, the story of John Snow and the Broad Street water pump looms large. In the 1800s, John Snow identified the water pump as the source of a cholera epidemic. He overcame community hesitancy and convinced those in charge to shut off the pump, bringing a swift end to the epidemic. The story is a great example of how information about the spread of a disease can be translated into an effective public health intervention. John Snow’s work also served as a catalyst for widescale investment in water sanitation. In keeping with this legacy, it is now time to do for airborne hazards what we once did for waterborne hazards. By taking a public health approach to airborne diseases and pollution through investments in indoor air quality, we can ensure a safer, healthier, more equitable, and more resilient society.
RELEVANT TERMSAdvanced Research Projects Agency for Health (ARPA-H): A new independent entity inside the National Institutes of Health (NIH), originally proposed by the Biden Administration and officially authorized in 2022, that aims to improve the US government’s ability to speed biomedical and public health solutions. Air filtration: The process of trapping particles on a filter to remove them from the air. Hierarchy of controls: A way of classifying and ranking safeguards against different types of hazards. High-efficiency particulate air filter (HEPA): An efficiency standard for a type of pleated air filter, commonly required to remove between 99.95 and 99.75 percent of small particles (diameter equal to 0.3 micrograms) that pass through the filter. Particulate matter (PM): Microscopic particles of solid or liquid matter suspended in the air, small enough to be inhaled and capable of causing serious health problems. Fine particulate matter, or PM2.5, refers to inhalable particles with diameters of 2.5 micrometers or smaller; these particles are especially harmful and are associated with increased risk of heart problems, asthma, low birth weight, and more. Universal design: The design of buildings, products, or environments to maximize their accessibility to a wide range of people, with and without disabilities. It is often contrasted with accommodations, which are specific exceptions that people with disabilities must request to make an otherwise inaccessible space or product usable. Ventilation: The process of moving air into, out of, or within a room, often but not necessarily pulling it through a filter while doing so. Ventilation rate: The rate at which fresh air is supplied to an indoor space, typically measured in liters per second (L/s) per person. Carbon dioxide levels are often used as proxies to gauge ventilation rates in occupied spaces. |
No comments:
Post a Comment