Why are UK resident doctors striking and what are they paid?
BBC July 14, 2025

Resident doctors in England are planning a walkout for five consecutive days from 25 July, over a pay dispute with the government.
They say they haven't had a "credible pay deal" for 2025-2026, but Health Secretary Wes Streeting argues the strike is "unreasonable" after substantial pay rises in recent years.Resident doctors in England to strike for five days in July
What are resident doctors' pay demands?
The British Medical Association (BMA), a trade union for doctors, says resident doctors' pay will be 20% lower in real terms than it was in 2008, even after an increase in August.
The BMA wants pay for the group - who used to be known as junior doctors - to be brought back in line with the level it was at 17 years ago, when they say their pay started to be eroded.
The claim is based on a measure of inflation called the Retail Price Index (RPI). This includes housing costs and shows higher price increases than some other inflation measures.
The BMA points out that many resident doctors have large student loans and that interest on these is calculated using RPI.
However, the government says RPI is outdated. Instead, it uses the Consumer Prices Index (CPI) to calculate inflation and pay increases. CPI looks at the cost of goods and services based on a basket of household items.
Using the CPI measure, the government says resident doctors' current pay is fair.
Analysis from the Nuffield Trust - a health think tank - suggests pay has fallen 5% since 2008 if CPI is used, compared with nearly 20% for RPI.
What pay rises have resident doctors had and what do they earn?
Since 2023, resident doctors have taken part in 11 separate strikes, arguing for fairer pay and working conditions.
During 2023-24, over two years, they received a 22% pay increase. From August this year, they will get an additional 5.4% pay rise.
Health Secretary Wes Streeting says resident doctors have received the largest pay rises of any public sector employees over the last three years.
The government says it won't be offering any further increases.
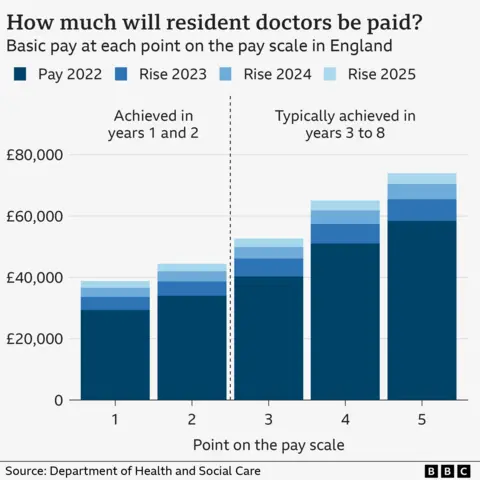
During their first foundation year after finishing their medical degree resident doctors in England earn a basic salary of £38,831, for an average of 48 hours worked per week. In the second year, this rises to £44,439.
Medics are often expected to work nightshifts, weekends and longer hours for extra payments.
After eight years as a resident doctor, salaries can progress to around £70,000.
What pay rises have people in other jobs had?
In May, the government announced pay rises for a number of public sector workers, including:4% for other doctors, dentists, and teachers in England, as well as prison officers in England and Wales
a 3.25% rise for civil servants
a 3.6% rise for some NHS staff in England, including nurses and midwives
a 4.5% rise for members of the UK armed forces, with 3.75% for senior military staff
However, the BMA argues that resident doctors may have built up more student debt than people working in other jobs.
A medical degree can take five or six years to complete - longer than most other degree courses.
Resident doctors also say they have little control on where and when they are asked to work. And it can be difficult to put down roots, because of the need to do placements in different parts of the country.
How will patients be affected by the resident doctors' strike?
The medics will stage a walkout in England from 07:00 on 25 July until 07:00 on 30 July.
NHS leaders have warned that patient care will be disrupted if the strike goes ahead.
On strike days, more senior doctors are likely to end up working in emergency and urgent care to replace striking resident doctors. As a result, many planned operations will have to be cancelled.
There were 507,000 appointments and operations cancelled and rescheduled because of strikes by doctors (some including consultants) between July 2023 and February 2024, according to government analysis.
Conservative leader Kemi Badenoch accused the prime minister of having "boasted that he solved the doctors' strike" only for them to take further action, adding that he'd been "weak" in dealing with the medics.
Scotland, Wales and Northern Ireland are not affected by these strikes.
Streeting to give UK doctors priority on NHS jobs, but won't boost pay offer
The Health Secretary is hoping to avoid damaging NHS strikes as he begins talks with the BMA this week

Wes Streeting is preparing to offer UK-trained doctors greater priority for NHS jobs as the Government scrambles to avert a fresh wave of strikes by resident doctors later this month.
The Government announced as part of its 10-year plan for the NHS that it would commit to hiring no more than one in ten NHS recruits from overseas, promising reform to a system where two-thirds of new doctors come from abroad.
However, The i Paper understands that ministers are now prepared to go further in negotiations with the British Medical Association (BMA) as they try to prevent resident doctors – formerly known as junior doctors – from going on strike.
In 2020, Matt Hancock expanded the competition for training posts to include applicants worldwide as the NHS faced a workforce shortage during the pandemic.
As a result, many more doctors are now competing for available jobs than there are positions, which slows their career progression.
The Government could offer to improve on tackling this bottleneck as part of negotiations on the strikes due to take place this week.
The Health Secretary is also said to be open to discussing other issues related to how annual leave and speciality rotations are managed.
Insiders have also insisted that Streeting’s proposal of cutting doctors’ pension pots to raise their pay is also still on the table, despite the BMA appearing to rule out this option publicly.
One insider said there was “enough common ground” to strike a deal on working conditions, even if the two sides remain divided on pay, and there were “lots of areas where we agree”.
Resident doctors are set to walk out between 25 and 30 July in a dispute over pay. The BMA is asking the Government to improve on its 5.4 per cent pay offer for this financial year, arguing that doctor pay is still 20 per cent lower in real terms than it was in 2008.
Ministers, however, have insisted they cannot budge on this offer, but are willing to make concessions on working conditions.
“While we cannot go further on pay this year, there is so much more we can do together to improve the lives of resident doctors and the wider NHS,” Streeting said in a letter to the BMA last week.
The conciliatory tone comes as insiders are increasingly concerned about the impact these strikes could have on the NHS, with warnings that NHS trusts are “in the dark” about how many trainee doctors could walk out.
Reports in The Sun on Sunday claim that unions have instructed doctors not to inform their hospitals of their intention to strike, which will make it harder for employers to plan adequate cover for the strikes.
Figures from NHS England show that during 44 days of walkouts in 2023, there was a 31 per cent drop in cancer operations and a 13 per cent drop in emergency heart surgery, with significant delays also reported in neonatal and mental health care.
During these strikes, many hospitals were aware of the number of doctors they needed to cover for, meaning the next round could have an even greater impact on service.
The British Medical Association has said it remains open to talks with the government to avert strike action later this month, but insists ministers have yet to make a “credible” offer.
While the union is willing to discuss “non-pay elements” that could help address doctors’ working conditions, it maintains that the dispute is fundamentally about pay erosion and that “not enough progress” has been made to restore the value of salaries.
In a letter sent to Health Secretary Wes Streeting on Friday, seen by The i Paper, the BMA wrote: “We are, as we have said, committed to meeting with you to settle our dispute and avoid strike action.”
However, it warned that “not only are you unwilling to talk about pay, but you have not identified any ‘non-pay’ issues for discussion either.” The union said it was “interested to know how you intend to resolve the dispute without any movement to address our pay erosion”.
The BMA also criticised the government for failing to deliver on previous commitments made in a deal last year, including on training rotations and exception reporting.
“The review into rotational training has barely got off the ground,” it wrote, adding that the small increases in training places announced in the NHS workforce plan “do not sufficiently address the immediate training bottleneck crisis”.
BIG READ
The NHS trust refusing to pay skilled staff an extra £1 an hour
A group of phlebotomists has been dubbed 'The Magnificent Thirty-Seven' after refusing to back down in the increasingly bitter stand-off with management at Gloucestershire Royal Hospital and Cheltenham General Hospital

An NHS trust stands accused of treating some of its lowest paid staff with contempt after denying them an extra £1 per hour in line with neighbouring hospitals.
A group of phlebotomists has been dubbed “The Magnificent Thirty-Seven” after refusing to back down in the increasingly bitter stand-off with management at Gloucestershire Royal Hospital and Cheltenham General Hospital.
The phlebotomists, healthcare professionals who take blood samples from patients to quickly diagnose diseases and conditions, have pent 107 days on strike making the industrial dispute one of the longest in NHS history.
The row centres around whether a national campaign to move healthcare support workers from band 2 to band 3 on the NHS pay scale should include phlebotomists. The Gloucestershire phlebotomists are currently band 2 and paid up to £12.51 an hour – 30p above the national minimum wage.
They argue that their knowledge, skills and training equate to those of a band 3 worker whose top tier is £13.60 – a £1.09 difference. The phlebotomists want to be regraded and given back pay to cover the extra duties they have been doing for years.
‘We want recognition’
Caroline Hayhurst, a former paramedic of 30 years who has been a phlebotomist at the trust for the last 10 years, said: “There are a number of trusts where staff are band 2 and the phlebotomy role does vary from trust to trust, but a lot of people are band 3 already and a lot of trusts have moved staff to band 3 on the back of our dispute. We know our skills align with band 3 and we want recognition of that.
“Ours is a very modest and justifiable claim. The patients are the ones that are inconvenienced the most yet they are telling us to stand our ground.”
The phlebotomists first raised concerns over their pay in February 2024 and submitted a formal complaint last September. Since then, they have accused the trust of ignoring a fair job-evaluation process and of attempting to avoid its obligation to properly assess their skills and responsibilities. The trust refutes the allegations.
The i Paper joined the phlebotomists as they attended the trust’s monthly public board meeting last Friday before returning to the picket line. After laying out the group’s concerns again, and to cheers from her colleagues, phlebotomist Kelly Carter asked the board: “Why are you continuously delaying, moving the goalposts and gaslighting us?”

The trust promised a job evaluation panel meeting will finally take place on 17 July when a decision will be made. After being told “the process remains ongoing” any further questions from the phlebotomists were shut down by the chair.
Speaking on the picket line following the meeting, Carter said: “It’s really hard to know that the trust has been blocking us. If we’d have had this meeting months ago we could have been back at work by now. It doesn’t feel like they’re thinking about the patients and we really want to get back and see them.
“We’re not asking for extra money – we’re asking them to look at our pay grade as we’re deserving of band 3. I came to this department to join this team. I used to be a receptionist and used to hear them all in their room and just wanted to be with them. We’ve been together so long and are so close that nothing is going to break us now. It’s gone past money, we’re fighting for justice.”
Hayhurst has acknowledged that some trusts continue to pay their phlebotomists on a band 2 rating, but points out that when the issue has been raised elsewhere, such as at the neighbouring Royal University Hospitals in Bath, as well as at trusts in Bristol, Dorset and Salisbury, managers have re-banded the role without the need for phlebotomists to resort to industrial action.
‘They want to save face’
“I don’t know whether it’s a principle now and they’re not willing to back down,” said Kelvin Willsher, 56, the sole man among The Magnificent Thirty-Seven. “Or, in my view, they’ve gone this far that they’re trying now to save face [by holding the evaluation panel]. I don’t know how they can live with themselves.”
Some of the phlebotomists have had to take time off work due to the stress of the situation, Willsher said. “Management say that they care, but the proof’s in the pudding. They don’t care.”
During their strike, the Gloucestershire phlebotomists’ work is being covered by band 4 and 5 nurses, which the phlebotomists argue supports their argument of it being a higher skilled role than band 2.
They are being supported by Unison as part of its pay fair for patient care campaign. Since 2021, more than 40,000 healthcare workers have received around £162m in back pay and more than £64m in salary increases as part of the union’s campaign.

Asked if they are prepared to strike indefinitely to achieve their aim, Hayhurst said: “Absolutely. This is more than just about money. This is about being valued in the role we perform, and it’s about future generations who want to stay in this job. Never before has there been such pressure on this, and to potentially throw our skills on the scrapheap and go and get a job in a factory because it pays more. Goodwill has run out.”
Kevin McNamara, chief executive of Gloucestershire Hospitals, has said he is “keen to stick within the national framework” so there is “fairness and consistency across the whole of the NHS”. He said the national campaign to move healthcare support workers from band 2 to band 3 did not include phlebotomists.
“I think it starts to undermine a pay terms and conditions framework if we start to take local decisions,” McNamara told the BBC this week.
He said he first asked union colleagues to share an updated job description for evaluation last autumn, but claimed he only received it two weeks ago. “It is something we’re committed to resolving but we have to do it in a proper process,” he said.
Unison general secretary Christina McAnea said: “Other NHS trusts in the region and elsewhere in the country are doing the right thing. They’re paying staff properly for the jobs they do, and compensating them fairly for extra work done previously.
“The bizarre, meanspirited approach adopted by senior executives at Gloucestershire is not only out of step with the rest of the NHS, it clearly isn’t working. There’s no reason why NHS workers in Gloucester and Cheltenham should settle for any less than the thousands of employees who’ve already seen their pay improved, thanks to their efforts and the union’s campaign.”
A trust spokesperson said: “As our phlebotomists have confirmed, our trust pays the same as most other NHS organisations in the country.
“The trust has asked Unison since October for a revised phlebotomy job description for review and they confirmed in March 2025 that there were no changes to the job description. However, they have since provided a revised job description, which was received on 27 June 2025. This week, the trust and Unison agreed that the evaluation panel will meet on 17 July to review the new job description.”
This comes as Health Secretary Wes Streeting will meet representatives from the British Medical Association (BMA) this week for talks in an effort to avoid planned strike action by resident doctors.
The i Paper understands that ministers are now prepared to go further in negotiations with the British Medical Association (BMA) as Streeting tries to prevent resident doctors – formerly known as junior doctors – from going on strike during this talks.
The BMA has said that resident doctors need a pay uplift of 29.2 per cent to reverse “pay erosion” since 2008-09. In September, BMA members voted to accept a government pay deal worth 22.3 per cent on average over two years.
The 2025-26 pay deal saw resident doctors given a 4 per cent uplift plus £750 “on a consolidated basis” – equating to an average pay rise of 5.4 per cent
No comments:
Post a Comment