The COVID pandemic has shown that public health in Europe relies massively on Asian supplies, from masks to antibiotics. EU attempts to reshore production seem to be going nowhere, and do they make sense, after all?
Insa Wrede
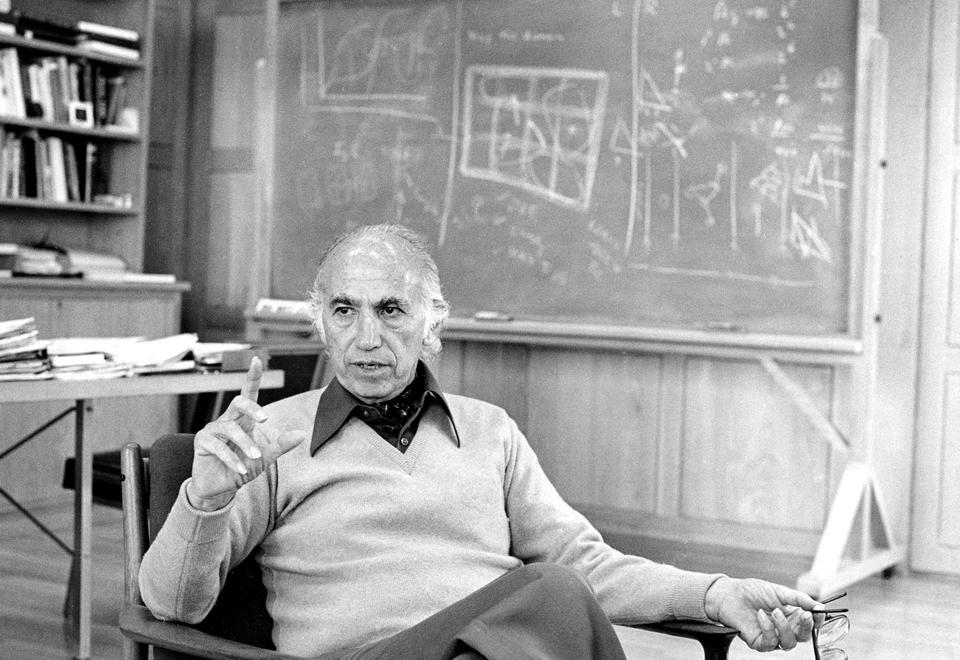
Ulrike Holzgrabe believes China wouldn't need an atomic bomb to deal a fatal blow to Europe. Just stopping its supplies of antibiotics would also do the trick, the professor for pharmaceutical and medicinal chemistry at Würzburg University in southern Germany told DW.
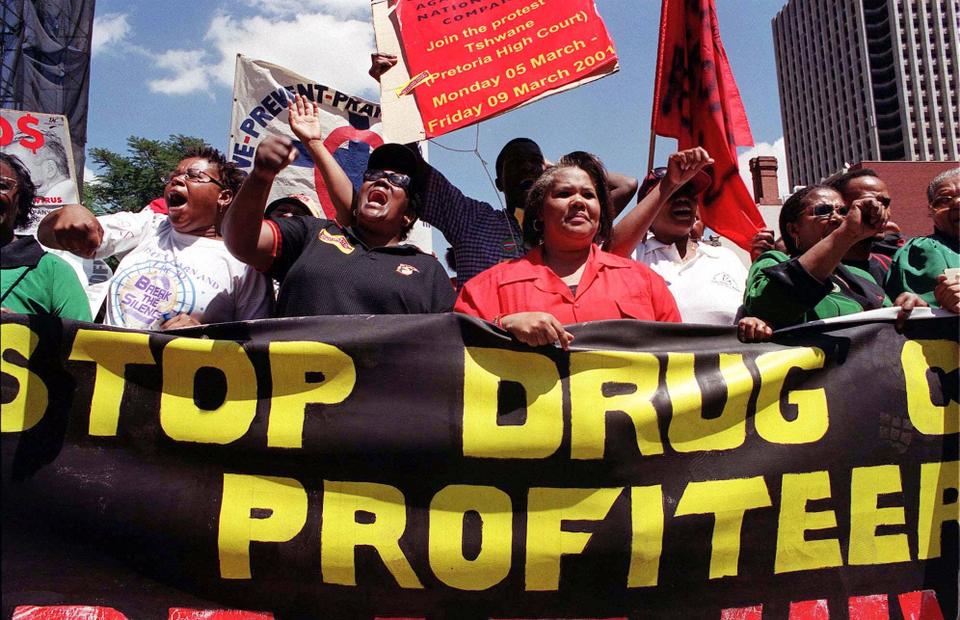
Europe's huge shortage of medical masks during the coronavirus pandemic has laid bare the continent's vulnerability to ensuring a steady supply of basic medicinal products. In 2020, the European Parliament stated in a report that public health could be a "geopolitical weapon that can bring down an entire continent."
The European Union has since attempted to identify the types of medicines it can only source from outside the bloc, notably from China. Holzgrabe said this effort needs to be intensified with a database on which company produces what and who provides the precursor chemicals for drug production.
Cut-throat competition and trade secrets
Establishing a precise pharmaceutical database is where the problem already begins, says Jasmina Kirchhoff from the German Economic Institute (IW) in Cologne, Germany. Information on the manufacturers of chemicals and other downstream ingredients are "well-kept trade secrets," the pharma business expert told DW.
It's critical for manufacturers to keep market advantages secret from competitors, especially in the generics sector. Generics are pharmaceutical drugs that contain the same chemical substance as a drug that was formerly protected by chemical patents.

The success of generic drugmakers depends on low prices, which means that supply chains are often "very complex, and making it unclear how many companies in which countries are involved," Kirchhoff said.
Regarding antibiotics, the IW researcher noted that China recognized "as early as the 1980s" how important it is to have its own antibiotic production. "There was massive investment in those factories that could produce at the lowest costs — first for the domestic market, and then the surplus output was exported," Kirchhoff added.
In addition to China, which has also become the largest producer of chemical precursor products for the global pharmaceutical market, India has emerged as a major supplier of pharmaceutical products.
National Pharma Strategy: Germany's reshoring initiative
As part of efforts to boost the domestic pharmaceutical industry, the German government adopted a strategy paper in December 2023 identifying three key areas to be strengthened. The goals include, first of all, unbureaucratic approvals for clinical trials with medicinal products. Secondly, easier access to health data for research purposes. And finally, incentives for setting up more manufacturing sites in the country.

Germany is still a major player in the global pharma market and home to leading companies such as Bayer, Boehringer Ingelheim and Merck Group. However, they are strong in the market for innovative, patented medications but weak in the generics market, said Holzgrabe, adding that generics production in Europe is hardly profitable due to low profit margins.
But generics are crucial for public health care in general, as they cover about 80% of basic medication needs, including many antibiotics.
Bork Bretthauer criticizes the government's strategy to boost domestic investments with subsidies. The CEO of Pro Generika — a German nonprofit that regularly commissions scientific studies into health policy and the pharma sector — told DW that Germany needs "a different pricing system" for drugs.
"We don't need zombie factories in Europe that need to be permanently subsidized," he said, adding that Europeans must be willing to pay higher drug prices.
Big Pharma needs big incentives
In the summer of last year, the German parliament adopted legislation aimed at incentivizing the German pharma industry to reshore production or at least stop relocating abroad, with higher drug prices. The law was also a result of drug shortages and supply bottlenecks that had emerged during the global pandemic and the Russian invasion of Ukraine.

It is a major healthcare policy change because Germany had sought to keep public health costs as low as possible until last year.
Previously, drugmakers were forced to offer statutory health insurance companies their medications at capped prices. So prices were fixed for about 80% of medications, including generic drugs, meaning that only the most cost-effective drug firms could make a profit.
Under the new legislation, insurance companies' drug tenders for specific active ingredients and off-patent medications must also award contracts to a European company.
Ulrike Holzgrabe believes the legislation is a step in the right direction, but fears it will come to nothing because there is "simply no European production left," especially in the generics sector. Jasmina Kirchhoff says the law has at least helped prevent more production from moving abroad.
China's unassailable dominance
Wolfgang Große Entrup, managing director of the Association of the German Chemical Industry (VCI), thinks higher drug prices are inevitable if Europe wants more security. But production in Europe will never be as cheap as in Asia, he said in April. The German pharma industry, in particular, would suffer from "excessive bureaucracy, skilled labor shortages, high energy costs, and crumbling infrastructure."
Holzgrabe shares this view, adding that Chinese drugmakers, by contrast, benefit from lower labor and energy costs and cost-free land allowances from the government when they establish production facilities. Moreover, they don't have to comply with environmental regulations as strict as those in Europe.
All of this, she said, would make it difficult to bring pharmaceutical production back to Europe so that "independence from China won't be achieved."
This article was originally written in German.










.png)


