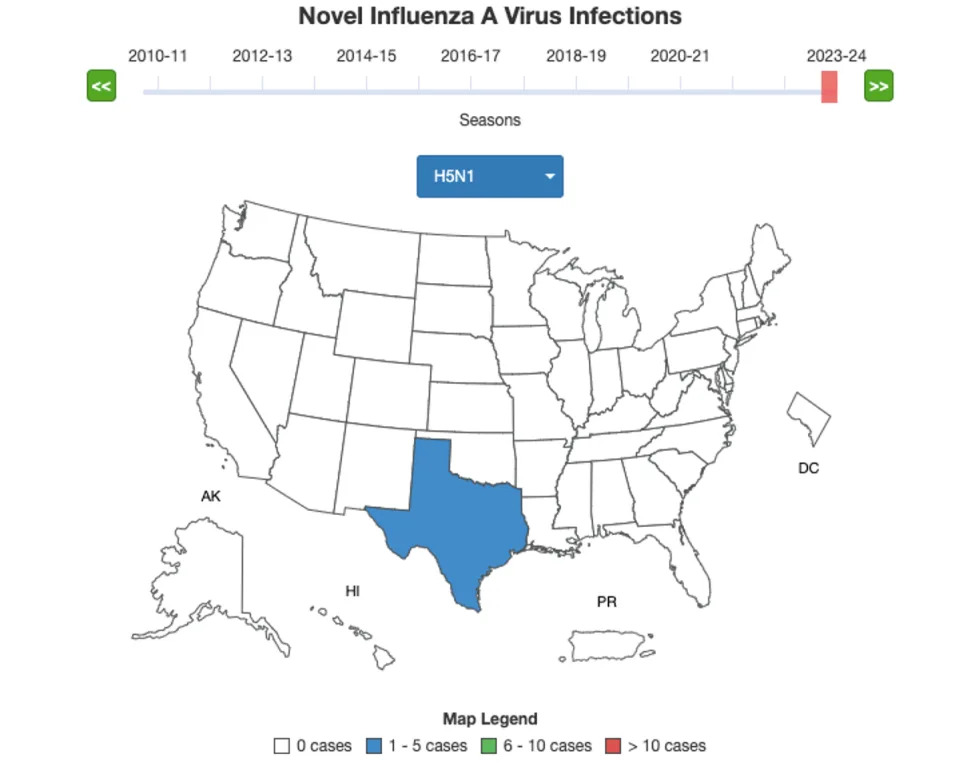
H5N1
Bird flu may now be spreading between humans, WHO fearsJoe Pinkstone
Fri, 24 February 2023

Bird flu vaccine Cambodia health security science ducks avian influenza - Tang Chhin Sothy/AFP via Getty Images
The World Health Organisation is “really concerned” the current bird flu outbreak may now be spreading between people for the first time in more than 25 years.
The WHO has ordered a new bird flu vaccine to be made in response to the rapid spread of the strain of H5N1 avian influenza causing the current outbreak.
An 11-year-old girl died of bird flu in Cambodia this week while her father is also infected and 11 others are under observation, with some showing symptoms. Experts are worried the large cluster might mean that the virus has now evolved to be able to be passed from one human to another.
While captive and wild birds have been decimated worldwide by the current H5N1 strain there has so far been no evidence that it can pass between mammals.
If the virus has been able to cross the species gap from birds to humans then concern around bird flu and its potential to cause a pandemic will escalate.
No sustained transmission of bird flu has ever occurred but limited human-to-human transmission was reported in Hong Kong in 1997.

experts - AFP
Dr Sylvie Briand, WHO director of epidemic and pandemic preparedness and prevention, said that the Cambodian outbreak was causing more alarm than isolated cases that have popped up in the intervening two decades.
“When you have only one case, you imagine that it's because this case was exposed to animals, either alive or dead. So for us it means it is a zoonotic infection,” she said on Friday.
“But when you see that there are a number of potential cases surrounding this initial case, you always wonder what has happened. Is it because maybe the initial case has transmitted the disease to other humans?
“And so we are really concerned about the potential human-to-human transmission coming from this initial spillover from animals.
“This is currently the investigation that is ongoing in the contacts of this girl in Cambodia. We are first trying to see if those contacts have H5N1 infection and that's why we are waiting for the laboratory confirmation of those cases.
“Secondly, once we have this confirmation, we will try to understand if those people have been exposed to animals or if those people have been contaminated by the initial case.”

Posters - Cambodia Ministry of Health
WHO staff have now been deployed on the ground in Cambodia and the results of these assessments will dictate the next steps.
Dr Richard Webby, director of the WHO Collaborating Centre for Studies on the Ecology of Influenza in Animals, added that “in response to the spread of H5N1 and a little bit of evolution” a new vaccine specifically against the currently dominant strain is now to be developed.
“We are putting another H5 virus vaccine candidate into production and that will start soon,” he said.
Dr Webby added that the current stockpile of candidate virus vaccines - which could be deployed into full-fledged jab drives should the animal infection be proven to have made the jump to spread among people - is also being assessed to see whether it works against the currently dominant form of bird flu.
Evidence suggests that if the current strain behind the ongoing avian pandemic did jump to people then the existing stockpile would work well against it, even if it may take six months to create the updated jab.
“There has been a little bit of work looking at some of the serum collected from people who took part in vaccine trials to some of these earlier H5 clades and several of those people actually worked quite well with some of the recently circulating viruses,” Dr Webby said.
“From a vaccine stockpile and response point of view, I think this is encouraging and suggests the human response to some of the vaccines does induce a broad immunity that cross-reacts with a lot of the clades we are seeing.”
Dr Wenqing Zhang, WHO Global Influenza Programme chief, added that there were almost 20 current H5 vaccines licensed for pandemic use, and the new one would add to this armoury.

chickens - Jamie McDonald/Getty Images
The WHO announcement comes after the UKHSA commissioned Covid-like modelling for bird flu should person-to-person transmission be found in the UK.
The UKHSA has activated a new technical group to create modelling for a potential human outbreak of bird flu, which includes Prof Neil Ferguson, who was instrumental in the first Covid lockdown in 2020, and UKHSA chief medical adviser Prof Susan Hopkins.
The UKHSA is also looking into bird flu lateral flow tests, documents show, as well as investigating what is the best lab-based test to pick up the virus.
A source close to the matter told the Telegraph that a host of permutations were being drawn up, including a U-shaped severity curve, akin to seasonal flu; a Covid-like scenario where the oldest and most frail are more likely to die; and the possibility that it is dangerous to all people, like Spanish flu.
One of the scenarios being investigated by officials is if the virus is relatively mild, with an infection fatality rate of 0.25 per cent, similar to Covid.
The most severe hypothesis is if the virus is as deadly in people as the 1918 Spanish flu pandemic, with a fatality rate of around 2.5 per cent, and a hospitalisation rate of one in 20.
Some estimates of bird flu’s fatality rate in humans are as high as 60 per cent but experts say this may be misleading and inflated by sampling bias from when H5N1 first emerged 20 years ago.
The modelling marks an escalation in preparedness by health authorities as the country’s worst ever bird flu outbreak continues to ravage poultry farmers and wild bird colonies alike.
Covid-style model for bird flu pandemic drawn up by health officials
Joe Pinkstone
Thu, 23 February 2023

Ducks gather at a farm in Snoa village outside Phnom Penh, Cambodia, Thursday, Feb. 23, 2023
- Heng Sinith
Health officials are drawing up Covid-esque modelling to see what would happen if the current bird flu pandemic evolved to be able to spread from human-to-human.
There is currently no evidence that the H5N1 avian influenza strain that has killed hundreds of thousands of birds in Britain can spread between mammals.
A nationwide housing order has been in place since November mandating that all captive birds be kept inside, which has led to a decrease in infections.
But the UKHSA has now activated a new technical group to create modelling for a potential human outbreak of bird flu.
The group features UKHSA’s own experts as well as some external academics who were prominent in the Covid response.
Health officials are drawing up Covid-esque modelling to see what would happen if the current bird flu pandemic evolved to be able to spread from human-to-human.
There is currently no evidence that the H5N1 avian influenza strain that has killed hundreds of thousands of birds in Britain can spread between mammals.
A nationwide housing order has been in place since November mandating that all captive birds be kept inside, which has led to a decrease in infections.
But the UKHSA has now activated a new technical group to create modelling for a potential human outbreak of bird flu.
The group features UKHSA’s own experts as well as some external academics who were prominent in the Covid response.
'Bird flu lateral flow tests'
The 26-person strong group includes UKHSA Chief Medical Advisor Prof Susan Hopkins; Imperial’s Prof Neil Ferguson, who has worked on bird flu for decades but is best known for his Spring 2020 projections which brought about the first Covid lockdown; and Prof Munir Iqbal, head of the Avian Influenza Group at The Pirbright Institute.
The UKHSA is also looking into bird flu lateral flow tests, documents show, as well as investigating what is the best lab-based test to pick up the virus.
“To facilitate preparedness, planning and improvements to surveillance, scenarios of early human transmission are being developed,” the UKHSA says in a technical briefing.
A source close to the matter told the Telegraph that a host of permutations are being drawn up, including a U-shaped severity curve, akin to seasonal flu; a Covid-like scenario where the oldest and most frail are more likely to die; and the possibility that it is dangerous to all people, like Spanish flu.
Models currently 'completely hypothetical'
The findings come after it was reported an 11-year-old girl died of bird flu in Cambodia and 12 other people have been infected.
Prof Iqbal said the UKHSA models were currently “completely hypothetical” as all available data indicates there is no ability for the virus to spread between people.
One of the scenarios being investigated by officials is if the virus is relatively mild, with an infection fatality rate of 0.25 per cent, similar to Covid.
The most severe hypothesis is if the virus is as deadly in people as the 1918 Spanish flu pandemic, with a fatality rate of around 2.5 per cent, and a hospitalisation rate of one in 20.
Some estimates of bird flu’s fatality rate in humans are as high as 60 per cent but experts say this may be misleading and inflated by sampling bias from when H5N1 first emerged 20 years ago.
The modelling marks an escalation in preparedness by health authorities as the country’s worst ever bird flu outbreak continues to ravage poultry farmers and wild bird colonies alike.
H5N1 now 'the world’s biggest pandemic threat'
Sir Jeremy Farrar, a former member of Sage and Chief Scientist designate of the World Health Organization, said the avian H5N1 virus is now the world’s biggest pandemic threat.
He called this week for governments to make vaccines against the virus as a precaution.
Amid the backdrop of the ongoing Covid Inquiry the news of fresh modelling for a potential viral outbreak is likely to cause alarm among both the public and policymakers.
The modelling from UKHSA will likely be key in deciding if any actions are required to curb spread, should the unlikely event of human-to-human transmission occur.

Colorized transmission electron micrograph of avian influenza A H5N1 viruses
- Phanie / Alamy Stock Photo
“The aims right now are to determine what level of surveillance we need to detect an event at an early stage,” a scientific source told The Telegraph.
“We haven't really seen very many people in Europe getting infected [with H5N1 avian influenza] and the people who have been infected have been very mildly ill or completely asymptomatic.
“It’s still H5N1 but it's evolved in enormous amount since it first emerged in Southeast Asia literally 20 years ago and it may have evolved more to be a virus which is well adapted at infecting a very wide range of species of birds, but less well adapted to infecting, certainly people, but maybe mammals.
“But we don’t know enough to be sure about that, which is why this work is going on but I think the risk is perhaps lower than it was.”
Scientists are concerned that with so much virus in birds, mammals are now more prone to eat an infected carcass and become infected that way. It is then possible that the virus evolves inside the infected mammals to be able to spread.
“The modelling right now is very focused on how much surveillance we need, in particular in hospitals which will pick up the severe cases, to be able to be sure that we can pick up an outbreak situation within a certain timescale,” a source said.
“There's no modelling of how bad the epidemic could be, or what we would do in terms of policy responses.”
“The aims right now are to determine what level of surveillance we need to detect an event at an early stage,” a scientific source told The Telegraph.
“We haven't really seen very many people in Europe getting infected [with H5N1 avian influenza] and the people who have been infected have been very mildly ill or completely asymptomatic.
“It’s still H5N1 but it's evolved in enormous amount since it first emerged in Southeast Asia literally 20 years ago and it may have evolved more to be a virus which is well adapted at infecting a very wide range of species of birds, but less well adapted to infecting, certainly people, but maybe mammals.
“But we don’t know enough to be sure about that, which is why this work is going on but I think the risk is perhaps lower than it was.”
Scientists are concerned that with so much virus in birds, mammals are now more prone to eat an infected carcass and become infected that way. It is then possible that the virus evolves inside the infected mammals to be able to spread.
“The modelling right now is very focused on how much surveillance we need, in particular in hospitals which will pick up the severe cases, to be able to be sure that we can pick up an outbreak situation within a certain timescale,” a source said.
“There's no modelling of how bad the epidemic could be, or what we would do in terms of policy responses.”