Jake Johnson, Common Dreams
August 31, 2023

Sen. Marsha Blackburn (R-TN) (Photo: X)
"Did a Big Pharma CEO write these talking points for you on the back of a campaign check?" one critic asked Republican Sen. Marsha Blackburn.
Polling data released this week shows that nearly 90% of Republican voters support allowing Medicare to negotiate drug prices directly with pharmaceutical companies.
But congressional Republicans—many of whom receive substantial funding from the pharmaceutical industry—have staked out the opposite position, bashing the Biden administration's rollout of the initial list of medications that will be subject to price negotiations and parroting drugmakers' arguments against the popular reforms.
"The Inflation Reduction Act's socialist drug price controls will stunt the development of lifesaving treatments and cures while granting the government more unnecessary control over Americans' lives," Sen. Marsha Blackburn (R-Tenn.) wrote on social media, invoking the well-worn and misleading narrative that curbing medicine costs would stifle innovation.
Blackburn received $215,500 in campaign donations from pharma and other health product PACs between 2017 and 2022, according to OpenSecrets.
"Did a Big Pharma CEO write these talking points for you on the back of a campaign check?" Tennessee State Rep. Gloria Johnson (D-90) wrote in response to Blackburn. (Johnson is currently exploring a U.S. Senate run against the Republican.)
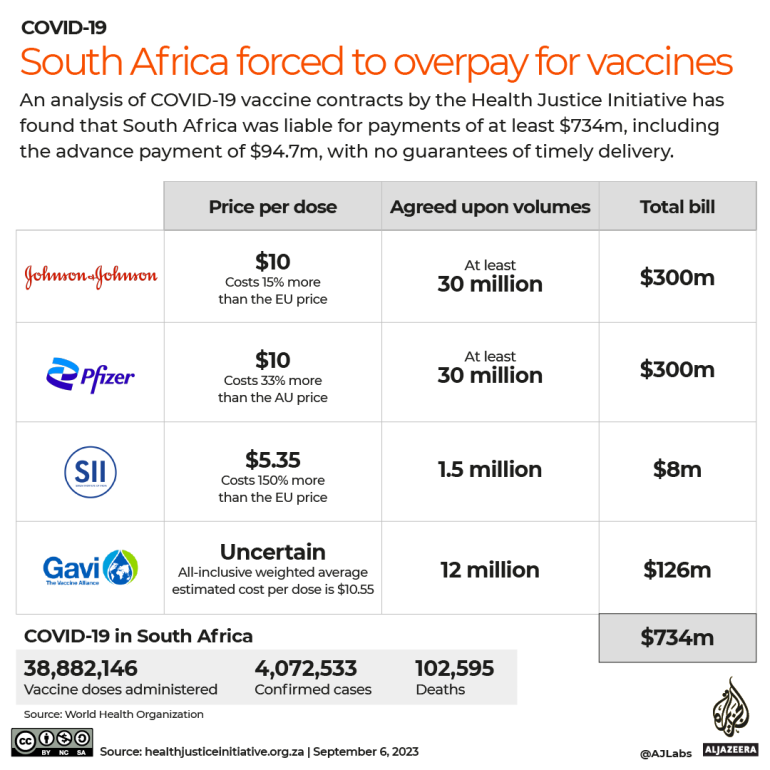
Every GOP lawmaker in the U.S. House and Senate voted against the Inflation Reduction Act (IRA), which requires Medicare to negotiate the prices of a subset of high-cost prescription drugs. After the legislation passed, Republicans swiftly began working to roll it back, taking specific aim at Medicare's new authority to negotiate drug prices, which are far higher in the U.S. than in other wealthy nations.
Republican presidential candidates—including former President Donald Trump, the frontrunner for the GOP nomination—have also vocally criticized the law and suggested they would work to repeal it if they win in 2024.
Earlier this week, the Centers for Medicare and Medicaid Services listed the first 10 drugs it plans to negotiate, drawing predictable backlash from the pharmaceutical industry, which lobbied against the IRA's passage and is now suing over the drug pricing provisions. Several of the drugs included on the initial list were already set to face generic competition in the coming years.
The Congressional Budget Office has estimated that the IRA's drug pricing reforms will save Medicare $160 billion over the next decade.
"Any effort by far-right Republicans to paint lowering the costs of prescription drug prices for Americans as a bad thing is laughable."
With President Joe Biden looking to make the drug price negotiations a centerpiece of his 2024 reelection campaign, Republican strategists are urging the GOP to aggressively counter the White House with messaging that mirrors industry claims about the IRA's potential impact on innovation—claims that advocates have long dismissed as false and self-serving.
"Republicans have to figure out how to go after it," Joe Grogan, a Republican strategist who served as a domestic policy adviser for Trump, toldPolitico. "They go after it by taking it head on: it is killing clinical programs, fundamentally restricting the amount of treatments."
Some GOP lawmakers are taking just that approach.
Sen. Mike Crapo (R-Idaho), whose campaign received $253,400 from pharma and health product PACs between 2017 and 2022, said in a statement Tuesday that Medicare price negotiations "risk reversing decades of progress on bringing lifesaving treatments and medical breakthroughs to American patients."
Rep. Jason Smith (R-Mo.), who has received donations from drug companies that are suing the Biden administration over the price negotiations, added that "the Biden administration is trying to take a victory lap while at the same time they are pricing seniors out of their healthcare and ensuring future cures never reach those who need them."
A 2021 report by Patients for Affordable Drugs concluded that "Big Pharma's innovation argument just does not stand up to scrutiny," noting that "the money that U.S.-based drug companies make by charging Americans high prices is 76% greater than what's needed to fund their entire global research and development expenditures."
Democrats have vowed to combat attempts by the pharmaceutical industry and Republicans to sabotage or repeal the IRA, which represents a modest effort to rein in drugmakers' power to drive up prices.
"The products that will now be subject to negotiation are used by millions of seniors in Medicare each year, costing each of them thousands of dollars," said Sen. Ron Wyden (D-Ore.), chair of the Senate Finance Committee. "I will be following the negotiation process closely and will fight any attempt by Big Pharma to undo or undermine the progress that's been made."
Rep. Raja Krishnamoorthi (D-Ill.) argued Wednesday that "any effort by far-right Republicans to paint lowering the costs of prescription drug prices for Americans as a bad thing is laughable."