By mid-May, all government hospitals will be occupied by infected patients, shows an estimate. India will fall short of infrastructure at the current rate of infections.
Pritam Datta, Chetana Chaudhuri 28 Mar 2020

Representational image. | Image Courtesy: YouTube
More than 5.49 lakh people around the world have been infected by the Novel Coronavirus, which has caused the Covid-19 pandemic. The pandemic has already claimed some 25,000 lives, and China and Italy have witnessed the worst of it. These two countries together account for 36% of infections and 53% of all worldwide deaths. India is in the early stages of this pandemic. By Friday, 27 March it had reported more than 770 Covid-19 cases and at least 20 deaths, and the graph of new infections, serious cases and fatalities is, as expected, constantly shifting.
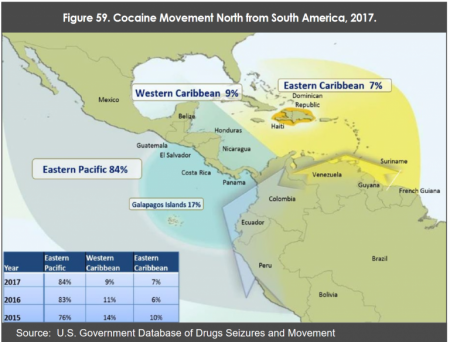
The case density in India of Covid-19 remains low, at 0.6 cases per million population. But cases are increasing at a faster rate (see Figure 1) now. The Indian government has taken several steps including quarantines, shutting the international borders, imposing social distancing and, finally, locking down the entire economy. Yet, at this crossroads for the whole human civilisation, the obvious question arises to what extent are Indians, who comprise 18% of world population, equipped to fight this pandemic. In other words, how long can Indians survive against this pandemic?
What we can learn from Italy and China’s health system is very relevant in this context.
Table 1: Outbreak of Novel Coronavirus in India
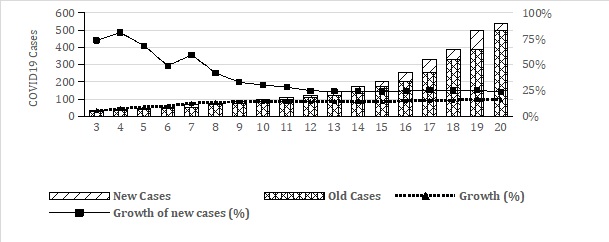 Source: Data sourced from https://covidout.in upto 22 March and thereafter, upto 25 March, from worldometers.info
Source: Data sourced from https://covidout.in upto 22 March and thereafter, upto 25 March, from worldometers.infoItaly and China are the two economies worst hit by the Covid-19 pandemic. They both have far more developed and well-equipped healthcare systems than India. As compared to India, Italy and China have a five-fold higher availability of hospital beds per lakh population. They also have, respectively, two and five times higher availability of physicians per lakh population as compared to India.
According to a press release issued by the Union Ministry of Health and Family Welfare 15.7 lakh beds are available in India’s public hospitals [July 2018] or 7 beds per million population. A study by the Indian Brand Equity Foundation [Page 10] estimates that the private sector accounts for 74% of hospitals and 40% of hospital beds in India. From this, one can conclude that India has 10.5 lakh beds available in private hospitals.
India may face a shortage of infrastructure to continue its battle against this global pandemic if the current rate of growth of Covid-19 positive cases continues for long.
Our estimate shows that by mid-May 2020, all government hospitals will be occupied by infected patients. All hospital beds, including private ones, are likely to be flooded by infected patients by the third week of May (see Table 2).
Table 2: Breakeven point for Indian Health Infrastructure (Hospital Bed) for Covid-19 treatment.
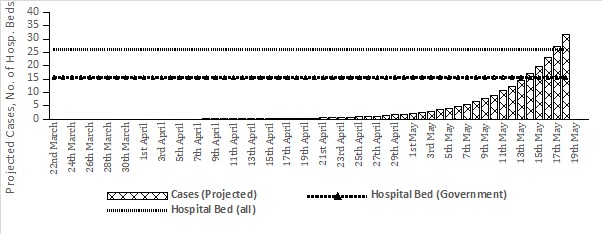 Source: Author’s own estimation, assuming 92% hospitalisation rate for Covid-19. [India’s Covid-19 recovery rate is roughly 7% and 1.9% is the death rate. Hence, a 92% hospitalisation rate has been assumed.
Source: Author’s own estimation, assuming 92% hospitalisation rate for Covid-19. [India’s Covid-19 recovery rate is roughly 7% and 1.9% is the death rate. Hence, a 92% hospitalisation rate has been assumed.As of 24 March 2020, the global gross mortality rate for Covid-19 is 4.5%. The gross mortality rate for the two worst-hit countries i.e. China and Italy, is 4% and 9.9% respectively. The mortality rate among Indian patients who were tested positive for Covid-19, is 1.9%, much less than the global Covid-19 mortality rate. [Gross mortality rate estimates are based on the number of deaths relative to the number of confirmed cases of Covid-19 infections.]
However, whereas the global average recovery rate from Covid-19 is 26% (in China and Italy, it is 90% and 12%), the average recovery rate of Indian Covid-19 patients is only 7% (See Table 1). This immediately implies an increase in the cumulative patient load. Hence, the only hope for India is its low case-density.
Table 3: Total Cases, Gross Morbidity, Recovery rate and case density of COVID-19
.png)
Source: https://www.worldometers.info/coronavirus/#countries (as on 25/03/2020)
There are 0.6 Covid-19 cases per million population in India, but the country also has low availability of hospital beds (7 per million population). It is clear that India, though it has slowed down the speed of fresh transmissions of the Novel Coronavirus, has no time to relax given the crisis situation countries such as Italy and China have faced.
One should not forget that though the death rate is lower in India as compared to Italy and China, the recovery rate is also lower in India.
This is primarily caused by the lack of infrastructure and manpower, which is represented by the number of hospital beds and health professionals in this study. Comparative analysis shows that the number of physicians, nurses and midwives and hospitals per lakh population are also very low in India as compared to Italy and China, and even compared to the world as a whole.
We should also not forget that the population in India is more than 22 times that of Italy. A majority of the labour force in India works in the informal sector. [The share of informal sector among male workers in 2017-18 was 71.1% and among female workers was nearly 54.8% in non-agriculture and AGEGC sectors (Periodic Labour Force Survey, Annual Report, 2017-18).]
Many of these workers have returned to their homes in rural areas from urban areas due to the lockdown of the economy. If infected, they would expose their family members and neighbours to the disease. In the absence of sufficient numbers of test-kits, this would pose a serious threat to the detection, isolation and treatment of people and further increase the chances of new infections.
In such a situation, locking down the country would marginally reduce the growth in the number of infected persons, but it would not provide a long-term solution to the pandemic. There is an urgent need to increase the number of hospitals, isolation wards and to provide for safety measures to health professionals as the infection spreads.
In spite of the reduction in speed of transmission, the number of infected persons is likely to exhaust India’s public health facilities, unless it is strengthened sufficiently, and quickly.
Pritam Datta is a fellow at the National Institute of Public Finance and Policy, New Delhi and Chetana Chaudhuri is a senior research associate at the Public Health Foundation of India (PHFI), Gurugram. The views are personal.
There are 0.6 Covid-19 cases per million population in India, but the country also has low availability of hospital beds (7 per million population). It is clear that India, though it has slowed down the speed of fresh transmissions of the Novel Coronavirus, has no time to relax given the crisis situation countries such as Italy and China have faced.
One should not forget that though the death rate is lower in India as compared to Italy and China, the recovery rate is also lower in India.
This is primarily caused by the lack of infrastructure and manpower, which is represented by the number of hospital beds and health professionals in this study. Comparative analysis shows that the number of physicians, nurses and midwives and hospitals per lakh population are also very low in India as compared to Italy and China, and even compared to the world as a whole.
We should also not forget that the population in India is more than 22 times that of Italy. A majority of the labour force in India works in the informal sector. [The share of informal sector among male workers in 2017-18 was 71.1% and among female workers was nearly 54.8% in non-agriculture and AGEGC sectors (Periodic Labour Force Survey, Annual Report, 2017-18).]
Many of these workers have returned to their homes in rural areas from urban areas due to the lockdown of the economy. If infected, they would expose their family members and neighbours to the disease. In the absence of sufficient numbers of test-kits, this would pose a serious threat to the detection, isolation and treatment of people and further increase the chances of new infections.
In such a situation, locking down the country would marginally reduce the growth in the number of infected persons, but it would not provide a long-term solution to the pandemic. There is an urgent need to increase the number of hospitals, isolation wards and to provide for safety measures to health professionals as the infection spreads.
In spite of the reduction in speed of transmission, the number of infected persons is likely to exhaust India’s public health facilities, unless it is strengthened sufficiently, and quickly.
Pritam Datta is a fellow at the National Institute of Public Finance and Policy, New Delhi and Chetana Chaudhuri is a senior research associate at the Public Health Foundation of India (PHFI), Gurugram. The views are personal.