International borders continue to hinder cross-border cooperation

Cross-border regions have great potential for cooperation, yet very few border regions are integrated, a new study from the University of Eastern Finland shows. Conducted by Dr. Francesco Cappellano and Professor Teemu Makkonen at the University of Eastern Finland's Karelian Institute, the study sheds light on the fact that although there is plenty of talk about promoting integration in cross-border regions, the reality is very different. In the border region of Cascadia that connects Seattle in the US with Vancouver in Canada, economic cooperation has been modest despite local decision-makers' high regard of it. The region has a long history of initiatives geared towards supporting cross-border cooperation, but visible results remain few and far between.
Published in Planning Practice & Research, the study was carried out within the Cross-Border Fellowship program funded by the Western Washington University in the US and the University of Victoria in Canada.
Cross-border cooperation has very little concrete evidence to show for
The study analyzed concrete outcomes of cross-border cooperation by using survey and statistical data. In particular, the researchers focused on innovation cooperation, i.e. cooperation in science, research and product development, as measured by the number of co-publications, co-patents and networking. The study shows that in Cascadia, the cross-border network of cooperation is very sparse, which can be seen in the scarcity of concrete collaborative scientific outcomes and patents. According to the researchers, this can be considered surprising.
"The economic profiles of Seattle and Vancouver are very similar, and increasingly close collaboration between the two is encouraged. This should foster cross-border cooperation, but it is still very seldom that partners are sought from across the border," Dr. Cappellano says.
The situation is not unique nor specific to border regions in North America alone. Professor Makkonen has observed similar development also in European border regions.
"Although cross-border cooperation in the European Union and in its adjacent areas is supported by, e.g., the Interreg and ENI programs, the outcomes have remained modest in terms of cooperation in science, research and product development. For instance, patents filed as a result of cross-border cooperation are rare."
Cross-border cooperation in the Öresund region connecting Sweden and Denmark is often regarded as a textbook example of well-functioning innovation cooperation. According to Professor Makkonen, however, this cooperation is not very impressive considering the resources, except in certain specific fields of medicine.
The findings of the study highlight the fact that although there is plenty of talk about promoting integration in cross-border regions, concrete outcomes remain few and far between.
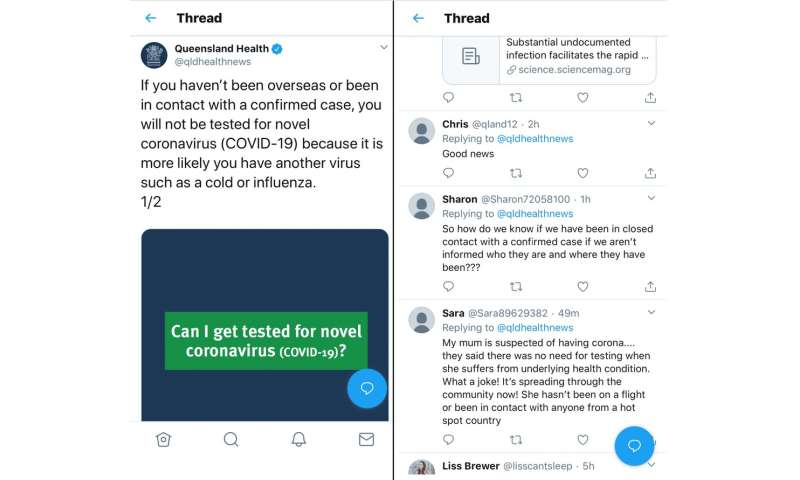
"The current relations between the EU and Russia, and the coronavirus pandemic, put the sustainability of cross-border cooperation to test. How to maintain cooperation even at current levels is a cause of concern," Professor Makkonen says.Russia to shut border with China over coronavirus
More information: Francesco Cappellano et al. The Proximity Puzzle in Cross-Border Regions, Planning Practice & Research (2020). DOI: 10.1080/02697459.2020.1743921
Provided by University of Eastern Finland