B.C. nurses, doctors cite protective equipment shortage, safety concerns
Ministry said ‘significant effort’ made to obtain sufficient protective gear
By Jeremy Hainsworth | May 5, 2020

iStock
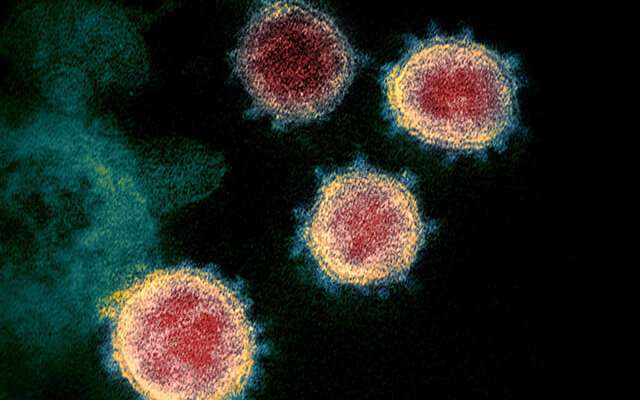
B.C.’s nurses and doctors have added their voices to those of those across the country who say there are insufficient amounts of personal protective equipment (PPE) for those on the frontline of the pandemic response.
“Nurses are getting only one mask per shift. Others have been told to leave their used mask on a piece of paper towel when they go on a break,” B.C. Nurses Union president Christine Sorensen said.
About 90% of doctors surveyed by the Canadian Medical Association April 28 indicated greater availability of PPE would help reduce their anxiety around the pandemic.
Indeed, Doctors of B.C. president Dr. Kathleen Ross said, “We have continuing concerns about supplies of PPE, understanding there is a worldwide shortage. These shortages aren’t just in hospitals, there is also a lack of access and supply for community based specialists and family physicians around the province.
“We have raised these concerns with the Ministry of Health and health authorities,” Ross said.
Provincial medical health officer Dr. Bonnie Henry has said currently postponed surgeries may be available this month.
But, said Ross, “when elective surgeries begin ramping up, additional pressure will be put on PPE supplies, which is causing additional concern.”
Sorenson said the union has received 1,700 complaints since March from nurses across B.C. health saying employers aren’t providing adequate numbers of gowns, gloves, face shields and N95 respirator masks. The union said the equipment is critical to protecting both nurses and their patients as the coronavirus pandemic continues.
Asked if there was a shortage of PPE, the Ministry of Health could not immediately answer.
“Healthcare workers are the frontline in our battle against COVID-19,”spokesperson Alex Peaker said. “They are responding courageously to monumental challenges during this unprecedented time. Their safety is our fundamental concern.
Peaker said the government “undertook a significant and active effort to acquire additional supply of personal protective equipment through all available options.”
As well, Peaker said, elective surgeries were postponed in preparation for COVID-19 and reduced hospital acute-care capacity to about 60%. “This protects healthcare workers, patients and the public.”
“We will continue to stand with and protect our healthcare workers, with the support of all British Columbians,” Peaker said.
Sorensen, however, questions what pandemic response measures or other disease transmission controls existed before the pandemic and how healthcare sector employers intend to respond as the pandemic continues.
“Respirators, masks and other PPE are meant to be the last line of defense for care providers, after all other control measures are in place,” Sorensen said. “The fact that some hospital emergency rooms still have triage desks without plexi-glass barriers, like the ones now present in grocery stores and food processing plants, is quite simply beyond me.”
Ross said PPE supplies are coordinated provincially through the Provincial Health Services Authority and distributed to health authorities.
Ross said doctors have been using virtual care options more often during the pandemic but said as restrictions ease, in-person care would increase creating a need for PPE in community practice.
“The process for acquiring PPE for community doctors is less clear than for those in facilities, as there is no real acquisition process yet in place, Ross said. “Community doctors are finding there is a lack of information about supply and most don’t know where to obtain PPE or who to ask.
She said discussions are ongoing as to where PPE can be sourced.
“ This will likely be through the emergency operations committees for each health authority,” Ross said. “We have asked health authorities to clarify this process.”
And, Ross explained, some health authorities are working with family practitioners but only in selected areas.
“This is a significant challenge, and we are working with the provincial government to develop plans that meet the needs of community doctors in a timely way,” Ross said.
Vancouver Coastal Health Authority and Fraser Health Authority referred questions to the ministry.
The B.C. Hospital Employers Association could not be immediately reached for comment.
jhainsworth@glaciermedia.ca
@jhainswo
VIEW COMMENTS