IANS
JUN 2, 2022, 12:26 IST
The monkeypox virus may be spreading 'undetected', said the World Health Organisation even as the global confirmed cases rise to more than 550 from 30 countries that are not endemic to the virus.
While, so far, most cases have been reported among men who have sex with men presenting with symptoms at sexual health clinics, "the sudden appearance of monkeypox in many countries at the same time suggests there may have been undetected transmission for some time," said WHO Director-General Tedros Adhanom Ghebreyesus, in a statement.
The virus may have been transmitted for months or years undetected though investigations are ongoing and there are clear no answers yet, added Dr. Rosamund Lewis, the WHO's monkeypox technical lead, during a news conference in Geneva.
"We don't really know whether it's too late to contain. What WHO and all member states are trying to do is prevent onward spread," Lewis said. Contact tracing and isolating patients who have monkeypox are crucial to stopping the spread, she said.
Earlier the WHO had refuted the need to avoid LGBTQ+ parades, as the virus itself is not a sexually transmitted infection, which are generally spread through semen and vaginal fluids.
"These communities are working hard to inform their members about the risks of monkeypox, and prevent transmission," Ghebreyesus said, adding the need to "work hard to fight stigma".
He noted that stigma against the LGBTQ+ community could "prevent infected individuals from seeking care, making it harder to stop transmission".
The global health body has also urged affected countries to widen their surveillance, to look for cases in the broader community.
Monkeypox has not previously been described as a sexually transmitted infection, but it can be passed on by direct contact during sex.
Anyone can be infected with monkeypox if they have close physical contact with someone else who is infected.
"The situation is evolving, and we expect that more cases will continue to be found," the WHO chief said.
While monkeypox symptoms resolve on their own, it "can also be severe in some cases".
Ghebreyesus said that the WHO is working to provide accurate information to those groups most at risk of monkeypox; to prevent further spread among at-risk groups; to protect frontline health workers; as well as to advance understanding of this disease.
Meanwhile, even as some countries are racing to stockpile smallpox vaccines against monkeypox, the WHO has not recommended mass vaccination.
But, the WHO is working with companies to increase access to those new vaccines and treatments, Lewis said.
The monkeypox virus may be spreading 'undetected', said the World Health Organisation even as the global confirmed cases rise to more than 550 from 30 countries that are not endemic to the virus.
While, so far, most cases have been reported among men who have sex with men presenting with symptoms at sexual health clinics, "the sudden appearance of monkeypox in many countries at the same time suggests there may have been undetected transmission for some time," said WHO Director-General Tedros Adhanom Ghebreyesus, in a statement.
The virus may have been transmitted for months or years undetected though investigations are ongoing and there are clear no answers yet, added Dr. Rosamund Lewis, the WHO's monkeypox technical lead, during a news conference in Geneva.
"We don't really know whether it's too late to contain. What WHO and all member states are trying to do is prevent onward spread," Lewis said. Contact tracing and isolating patients who have monkeypox are crucial to stopping the spread, she said.
Earlier the WHO had refuted the need to avoid LGBTQ+ parades, as the virus itself is not a sexually transmitted infection, which are generally spread through semen and vaginal fluids.
"These communities are working hard to inform their members about the risks of monkeypox, and prevent transmission," Ghebreyesus said, adding the need to "work hard to fight stigma".
He noted that stigma against the LGBTQ+ community could "prevent infected individuals from seeking care, making it harder to stop transmission".
The global health body has also urged affected countries to widen their surveillance, to look for cases in the broader community.
Monkeypox has not previously been described as a sexually transmitted infection, but it can be passed on by direct contact during sex.
Anyone can be infected with monkeypox if they have close physical contact with someone else who is infected.
"The situation is evolving, and we expect that more cases will continue to be found," the WHO chief said.
While monkeypox symptoms resolve on their own, it "can also be severe in some cases".
Ghebreyesus said that the WHO is working to provide accurate information to those groups most at risk of monkeypox; to prevent further spread among at-risk groups; to protect frontline health workers; as well as to advance understanding of this disease.
Meanwhile, even as some countries are racing to stockpile smallpox vaccines against monkeypox, the WHO has not recommended mass vaccination.
But, the WHO is working with companies to increase access to those new vaccines and treatments, Lewis said.
Monkeypox: Young men in London make up majority of UK cases, new data reveals
JUNE 2, 2022
PINK NEWS
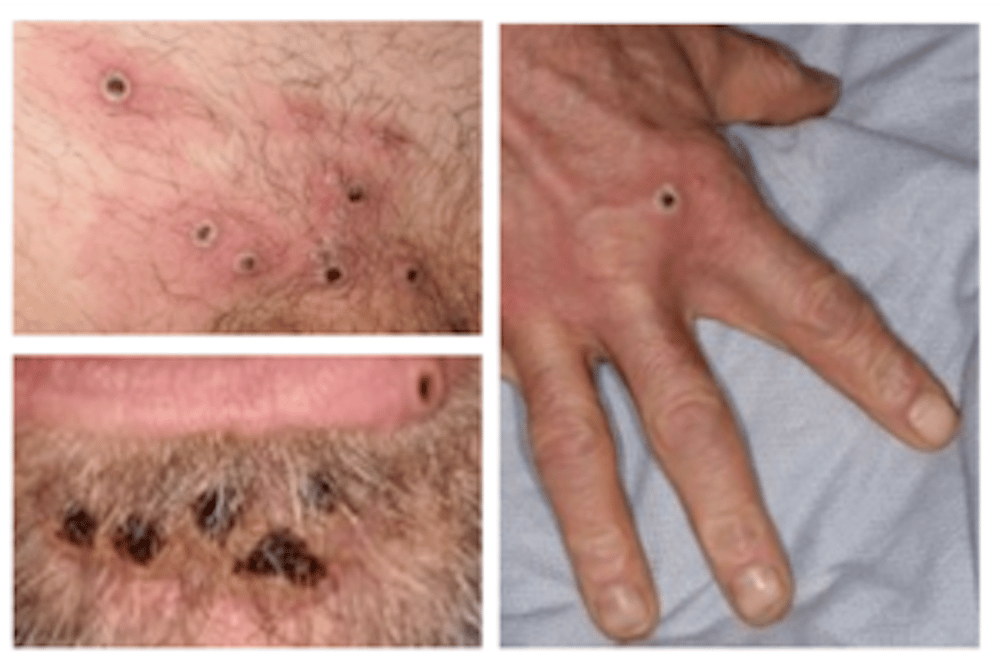
Monkeypox lesions. (UKHSA)
Young men living in London are making up the majority of UK monkeypox cases, new data has revealed.
The total number of confirmed monkeypox cases in the UK has now passed 200, with 199 cases in England, five in Scotland, two in Northern Ireland and one in Wales, as of Thursday (2 June)
On Wednesday (1 June), the UK Health Security Agency (UKHSA) released more information about the populations affected by monkeypox.
Although monkeypox can affect anyone, of the 190 UK cases confirmed from 6 to 30 May, more than half (111) were among men who have sex with men. Just two of those infected were women.
In England, 86 per cent of cases were detected in London, and almost all of those infected (87 per cent) were young, from 20 to 49 years old. Travel to other European countries within the three weeks before diagnosis was only reported in 18 per cent of cases.
So far, UKHSA investigations have “identified links to gay bars, saunas and the use of dating apps in the UK and abroad”, the agency said.
It said it was working with LGBTQ+ organisations like the Terrence Higgins Trust, Stonewall and Grindr, as well as with the British Association of Sexual Health and HIV (BASHH) and the British HIV Association, to provide queer communities with public health information about monkeypox. The LGBT Consortium and Pride organisers have also been asked to share this information.
However it said the UKHSA would continued to investigate, as “currently no single factor or exposure that links the cases has been identified”.
Last month, the UK purchased 20,000 doses of the Imvanex vaccine, a smallpox vaccine that has has proved to be about 85 per cent effective in preventing monkeypox, according to the World Health Organization (WHO).
The vaccine is being offered to people who have had contact with a confirmed case of monkeypox, as well as to healthcare workers.
Dr Meera Chand, director of clinical and emerging infections at UKHSA, said: “We are working to break chains of transmission, including by contact tracing and vaccination.
“We are grateful to everyone who has come forward for testing and it is extremely important that everyone continues to be aware of the symptoms and to seek advice if they have concerns.
“We are reminding people to look out for new spots, ulcers or blisters on any part of their body. If anyone suspects they might have monkeypox, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person.”
PINK NEWS
Monkeypox lesions. (UKHSA)
Young men living in London are making up the majority of UK monkeypox cases, new data has revealed.
The total number of confirmed monkeypox cases in the UK has now passed 200, with 199 cases in England, five in Scotland, two in Northern Ireland and one in Wales, as of Thursday (2 June)
On Wednesday (1 June), the UK Health Security Agency (UKHSA) released more information about the populations affected by monkeypox.
Although monkeypox can affect anyone, of the 190 UK cases confirmed from 6 to 30 May, more than half (111) were among men who have sex with men. Just two of those infected were women.
In England, 86 per cent of cases were detected in London, and almost all of those infected (87 per cent) were young, from 20 to 49 years old. Travel to other European countries within the three weeks before diagnosis was only reported in 18 per cent of cases.
So far, UKHSA investigations have “identified links to gay bars, saunas and the use of dating apps in the UK and abroad”, the agency said.
It said it was working with LGBTQ+ organisations like the Terrence Higgins Trust, Stonewall and Grindr, as well as with the British Association of Sexual Health and HIV (BASHH) and the British HIV Association, to provide queer communities with public health information about monkeypox. The LGBT Consortium and Pride organisers have also been asked to share this information.
However it said the UKHSA would continued to investigate, as “currently no single factor or exposure that links the cases has been identified”.
Last month, the UK purchased 20,000 doses of the Imvanex vaccine, a smallpox vaccine that has has proved to be about 85 per cent effective in preventing monkeypox, according to the World Health Organization (WHO).
The vaccine is being offered to people who have had contact with a confirmed case of monkeypox, as well as to healthcare workers.
Dr Meera Chand, director of clinical and emerging infections at UKHSA, said: “We are working to break chains of transmission, including by contact tracing and vaccination.
“We are grateful to everyone who has come forward for testing and it is extremely important that everyone continues to be aware of the symptoms and to seek advice if they have concerns.
“We are reminding people to look out for new spots, ulcers or blisters on any part of their body. If anyone suspects they might have monkeypox, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person.”















.png)




