7 hours ago
By Aurelia Foster
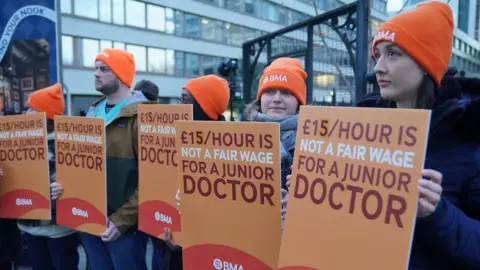
Junior doctors in England will strike on five days from 24 to 28 February, in an ongoing dispute with the government about pay.
The British Medical Association (BMA), which represents junior doctors, wants a 35% pay increase - a proposal previously rejected by ministers.
Many routine hospital services are likely to be disrupted or cancelled.
The government said it wanted to find a "reasonable solution" and is prepared to "go further" on a pay offer.
Junior doctors received a pay rise averaging nearly 9% this financial year - and during talks at the end of 2023, the option of an extra 3% on top of that was discussed.
But those talks ended in early December without a deal being reached.
The BMA said the government had "failed to to meet the deadline to put an improved pay offer on the table".
Junior doctors committee co-chairs Dr Robert Laurenson and Dr Vivek Trivedi said: "We have made every effort to work with the Government in finding a fair solution to this dispute whilst trying to avoid strike action."
They added that they believed the forthcoming strike could still be called off if a "credible offer" was made.
The BMA previously said the pay increase it was calling for would make up for what it said had been below-inflation rises since 2008.
Health secretary Victoria Atkins said: "This action called by the BMA Junior Doctor Committee does not signal that they are ready to be reasonable.
"We urged them to put an offer to their members, but they refused.
"Five days of action will put enormous pressure on the NHS and is not in the spirit of constructive dialogue."
This will be the 10th strike by junior doctors since March 2023. It will follow a six-day strike by junior doctors in January, the longest in the history of the NHS, which saw about 100,000 appointments cancelled.
Nearly half of NHS doctors are junior doctors - a group that spans those just out of university through to some who have 10 years or more experience.
The BMA is also balloting junior doctors on further industrial action beyond this strike.
More than 1.2 million medical appointments have been cancelled since December 2022, due to strikes by NHS workers, including nurses, paramedics and consultants.
The union is currently in talks with the government about a fresh pay deal for consultants, after rejecting the most recent offer.
‘Culture of fear’ at hospital where junior surgeons assaulted, report finds
A surgeon physically assaulted two trainees at a Brighton hospital during an operation, a fresh report has revealed.

(Gareth Fuller/PA)
By Anahita Hossein-Pour, PA
A review by the Royal College of Surgeons discovered instances of bullying and harassment at the Royal Sussex County Hospital, and a further “culture of fear” regarding the top leadership team.
Bosses at University Hospitals Sussex NHS Foundation Trust, which runs the hospital, commissioned the investigation into its surgery services which took place in May 2023.
It was apparent to the review team that there was a feeling of relative hopelessness within the general surgery department and it was clear that these reputational and cultural issues had affected the morale of many passionate and committed members of staff, some of whom had worked in the trust for 20-30 yearsThe Royal College of Surgeons
The Royal College of Surgeons flagged serious concerns between surgical staff and the trust’s senior leadership and said whistleblowers were poorly treated, such as by being bullied or subjected to disciplinary action.
They said: “There were concerning reports of bullying by members of the executive leadership team, with instances of confrontational meetings with individual consultant surgeons, when they were told to “sit down, shut up and listen”, with no ability to express their own concerns, and where they were alone and outnumbered.
“It was apparent to the review team that there was a feeling of relative hopelessness within the general surgery department and it was clear that these reputational and cultural issues had affected the morale of many passionate and committed members of staff, some of whom had worked in the trust for 20-30 years.”
The team also discovered a “dysfunctional” team working within the general surgery department and surgical teams, and were told consultant surgeons were “dismissive and disrespectful” towards other staff.
They added: “Reports of negative culture and behaviours within the general surgery department and wider trust was of concern to the review team.

The report comes as Sussex Police detectives are investigating the deaths of around 40 people at the Royal Sussex County Hospital due to allegations of medical negligence (Jonathan Brady/PA)
“It is imperative that robust action is taken to tackle unacceptable behaviours, given the reports of bullying, harassment and physical abuse.”
Major concerns were also raised over high cancellations of planned surgery for patients, often on the day and after patients had been waiting up to seven hours without eating or drinking ahead of their operation.
They added: “The review team heard about patients being cancelled multiple times and this was causing patients psychological distress.”
The findings come as Sussex Police detectives are investigating the deaths of around 40 people at the Royal Sussex County Hospital due to allegations of medical negligence.
The claims relate to concerns over neurosurgery and general surgery between 2015 and 2021.
In the conclusions from the Royal College of Surgeons, it said the team found staff who were interviewed in their probe “extremely engaged, open and helpful”, adding: “Within the constraints of current challenges they were facing, it was clear that staff worked very hard to offer the best possible service for their patients.”
Long-term problems cannot be solved overnight but significant strides are now being madeDr George Findlay
The appointment of the chief of surgery was also highlighted as a positive step, with the new boss described as attentive and responsive when staff escalated concerns.
The trust’s chief executive Dr George Findlay said he asked for this independent report because of the “huge challenges” the surgery teams have faced over many years and that all trust staff are focused on improving care.
Dr Findlay said: “Since last May when the review took place, major changes have begun – we have invested in extra staff and are recruiting now, we are seeking more theatre and bed capacity, and we have approved the opening of a Surgical Assessment Unit.
“The reviewers also noted the open attitude of staff and good local leadership – essential ingredients for a good service.
“Long-term problems cannot be solved overnight but significant strides are now being made. We all want to further improve patient care, so the job of building a stronger structure around the team, and stronger relationships, remains an absolute priority.”
The report, which was published on January 17, is set to be discussed by the trust’s board of directors on February 8.

 Senior vice principal Prof Karl Leydecker recommended the changes to the university court
Senior vice principal Prof Karl Leydecker recommended the changes to the university court