Are microwaves the answer?
by Cardiff University
Provided by Cardiff University
by Cardiff University
DECEMBER 4, 2020
Credit: Cardiff University
Researchers from Cardiff University have been testing the feasibility of using microwave ovens and dry heat to decontaminate crucial PPE being used to combat the coronavirus pandemic.
Reporting their findings in the Journal of Hospital Infection, the team have shown that certain types of respirators can be effectively decontaminated in just 90 seconds using an industrial-grade microwave oven and a baby bottle sterilizer containing water.
It has been widely reported that access to respirators and surgical face masks has become restricted in many facilities over the course of the pandemic.
"Being unable to access adequate PPE puts frontline workers and patients at risk of contracting coronavirus. Whilst masks are usually considered to be single use items, we wanted to find out whether they could be safely disinfected and used again," said co-author of the study Prof Jean-Yves Maillard, from the School of Pharmacy and Pharmaceutical Sciences.
The researchers believe microwave decontamination could be used in emergency situations to address supply issues and dramatically increase the number of respirators available to frontline staff.
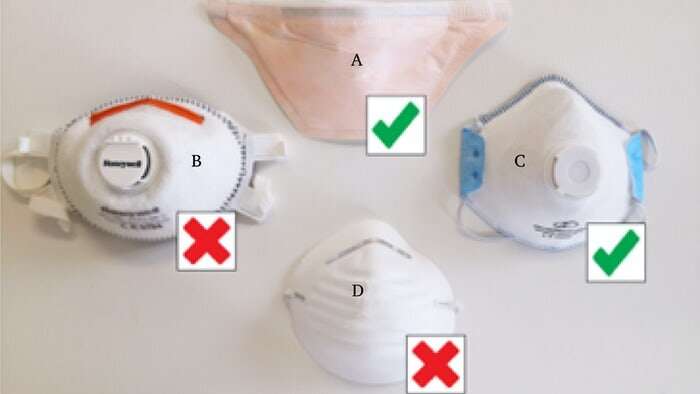
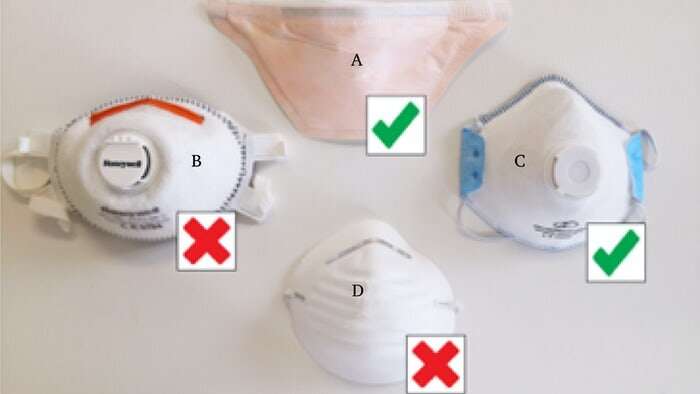
In the study, respirators were exposed to three microwave disinfection cycles and were shown to retain their ability to filter bacteria and viral-sized aerosols. However, the researchers reported that microwaving surgical masks led to a complete loss of their aerosol filtering capacity.
Michael Pascoe, co-author of the study from the School of Pharmacy and Pharmaceutical Sciences, said: "Surgical masks are known to lose effectiveness once they become moist—we suspected that microwave disinfection would lead to a similar loss in their ability to filter aerosols and this was confirmed by our lab observations."
The team, which also includes academics from the School of Engineering, also investigated using dry heat ovens as an alternative approach. Dry heat sterilization does not involve any water and so is compatible with items which are damaged by moisture.
Exposure to 70°C dry heat for 90 minutes was effective at decontaminating both surgical masks and respirators. After three dry heat cycles, both types of mask retained their aerosol filtering properties.
It is essential that PPE is effectively decontaminated between uses. Whilst microwave-generated steam and dry heat have both been shown to effectively kill coronaviruses, the researchers wanted to ensure that this method was also effective against bacteria encountered in healthcare environments.
In the study, respirators and surgical masks were purposely contaminated with Staphylococcus aureus, a bacterial species highly prevalent in human airways which can cause soft tissue infections and sepsis. Staphylococcus aureus is also the accepted biological indicator to test the integrity of a mask.
Both methods effectively reduced the number of bacteria on masks to a safe level.
As a result of the study, the team have developed a protocol to determine which types of PPE would be suitable for different treatments with dry heat incubators or microwave ovens.
"Mask and respirator models vary considerably and so it is important to ensure the method of decontamination does not compromise their function."
The team warns against members of the public using a similar approach at home. Professor Adrian Porch, from the School of Engineering, said: "Domestic microwave ovens typically have much lower power, around 800 W, and use rotating turntables rather than a rotating antenna. Significantly longer exposure times would be needed to achieve similar results and it is unknown how this would affect the functioning of the mask. Masks which contain thin wires can even catch fire when placed in a microwave."
Explore further
Researchers from Cardiff University have been testing the feasibility of using microwave ovens and dry heat to decontaminate crucial PPE being used to combat the coronavirus pandemic.
Reporting their findings in the Journal of Hospital Infection, the team have shown that certain types of respirators can be effectively decontaminated in just 90 seconds using an industrial-grade microwave oven and a baby bottle sterilizer containing water.
It has been widely reported that access to respirators and surgical face masks has become restricted in many facilities over the course of the pandemic.
"Being unable to access adequate PPE puts frontline workers and patients at risk of contracting coronavirus. Whilst masks are usually considered to be single use items, we wanted to find out whether they could be safely disinfected and used again," said co-author of the study Prof Jean-Yves Maillard, from the School of Pharmacy and Pharmaceutical Sciences.
The researchers believe microwave decontamination could be used in emergency situations to address supply issues and dramatically increase the number of respirators available to frontline staff.
In the study, respirators were exposed to three microwave disinfection cycles and were shown to retain their ability to filter bacteria and viral-sized aerosols. However, the researchers reported that microwaving surgical masks led to a complete loss of their aerosol filtering capacity.
Michael Pascoe, co-author of the study from the School of Pharmacy and Pharmaceutical Sciences, said: "Surgical masks are known to lose effectiveness once they become moist—we suspected that microwave disinfection would lead to a similar loss in their ability to filter aerosols and this was confirmed by our lab observations."
The team, which also includes academics from the School of Engineering, also investigated using dry heat ovens as an alternative approach. Dry heat sterilization does not involve any water and so is compatible with items which are damaged by moisture.
Exposure to 70°C dry heat for 90 minutes was effective at decontaminating both surgical masks and respirators. After three dry heat cycles, both types of mask retained their aerosol filtering properties.
It is essential that PPE is effectively decontaminated between uses. Whilst microwave-generated steam and dry heat have both been shown to effectively kill coronaviruses, the researchers wanted to ensure that this method was also effective against bacteria encountered in healthcare environments.
In the study, respirators and surgical masks were purposely contaminated with Staphylococcus aureus, a bacterial species highly prevalent in human airways which can cause soft tissue infections and sepsis. Staphylococcus aureus is also the accepted biological indicator to test the integrity of a mask.
Both methods effectively reduced the number of bacteria on masks to a safe level.
As a result of the study, the team have developed a protocol to determine which types of PPE would be suitable for different treatments with dry heat incubators or microwave ovens.
"Mask and respirator models vary considerably and so it is important to ensure the method of decontamination does not compromise their function."
The team warns against members of the public using a similar approach at home. Professor Adrian Porch, from the School of Engineering, said: "Domestic microwave ovens typically have much lower power, around 800 W, and use rotating turntables rather than a rotating antenna. Significantly longer exposure times would be needed to achieve similar results and it is unknown how this would affect the functioning of the mask. Masks which contain thin wires can even catch fire when placed in a microwave."
Explore further
Electric cooker an easy, efficient way to sanitize N95 masks, study finds
More information: M.J. Pascoe et al. Dry heat and microwave-generated steam protocols for the rapid decontamination of respiratory personal protective equipment in response to COVID-19-related shortages, Journal of Hospital Infection (2020). DOI: 10.1016/j.jhin.2020.07.008
More information: M.J. Pascoe et al. Dry heat and microwave-generated steam protocols for the rapid decontamination of respiratory personal protective equipment in response to COVID-19-related shortages, Journal of Hospital Infection (2020). DOI: 10.1016/j.jhin.2020.07.008
Provided by Cardiff University
No comments:
Post a Comment