Vaccination guards against certain bacterial infections and slows the spread of superbugs in populations
Vaccines that boost immunity against bacteria can protect the immunized from contracting drug-resistant infections, according to a team of scientists in the U.K. who also underscore that the shots can slow the spread of resistant strains in populations.
Scientists who developed a four-pronged mathematical model to better understand the impact of vaccination on antimicrobial resistance also found that while vaccination can prevent drug resistance, ironically, it also can help promote it in populations. What's needed is the right kind of vaccination strategy to keep resistant strains at bay, the scientists say.
The British team modeled the dynamics of vaccination and drug resistance across 27 European countries to draw a series of new conclusions about vaccination and its relationship on the control and spread of superbugs.
This startling way of understanding the drivers of drug resistance hails from the research of Dr. Nicholas Davies of the London School of Hygiene and Tropical Medicine. He and co-author, Dr. Katherine Atkins and a team of scientists, developed a modeling system that takes into account the diversity of bacterial species and competition among them as reasons for the evolution of drug resistant strains.
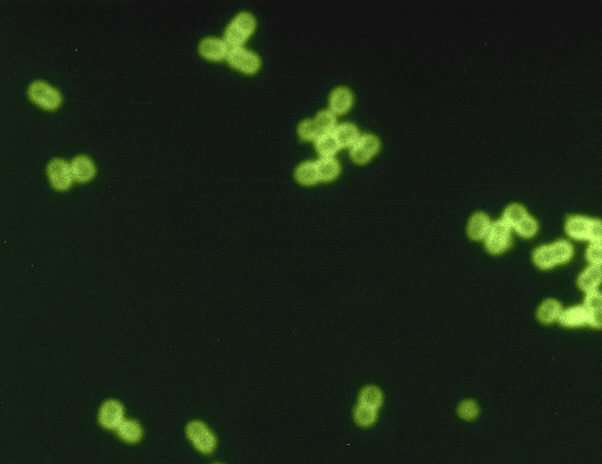
Writing in Science Translational Medicine Davies, Atkins and collaborators examined penicillin consumption and penicillin "nonsusceptibility"—resistance in Streptococcus pneumoniae—across the 27 countries. Their mathematical modeling shows how antibiotic-sensitive and antibiotic-resistant bacterial strains of Streptococcus pneumoniae—also known as pneumococcal bacteria—frequently co-exist in populations. Vaccination strategies have to be undertaken carefully to avoid tipping the balance in favor of superbug spread, they say.
"Competition and diversity are key to antibiotic resistance evolution and determine whether vaccines will prevent or increase resistant infections," Davies and colleagues assert.
Strep pneumoniae is a common and pervasive microbe that can invade many parts of the body causing serious, sometimes life-threatening infections. It can infiltrate the lungs, where it causes pneumococcal pneumonia; the ears, where it manifests as otitis media, the cause of infectious earaches; the nasal passages, where it gives rise to sinusitis; the blood, where the dangerous infection known as bacteremia can occur. Pneumococcus also can cause brain and spinal cord infections, diagnosed as bacterial meningitis.
Like Davies and his research group, teams of scientists worldwide have tackled the impact of pneumococcal vaccines on drug-resistant pneumococcal strains. A key to understanding many of these studies has been grasping this point: Having only limited pneumococcal vaccinations within a population can tip the balance in favor of increased pneumococcal infections among both children and adults and excessive use of antibiotics. This, in turn, gives rise to enhanced opportunities for the evolution—and spread—of tough-to-fight drug resistant strains. In short, more people wind up being treated with antibiotics rather than avoiding them. Excessive use of antibiotics is a driver of drug resistance.
"Vaccines against bacterial pathogens can protect recipients from becoming infected with potentially antibiotic-resistant pathogens. However, by altering the selective balance between antibiotic-sensitive and antibiotic-resistant bacterial strains, vaccines may also suppress—or promote the spread of antibiotic resistance—among unvaccinated individuals," the Davies team wrote.
Atkins said the research lays the groundwork for a better understanding of the dynamics between vaccines and drug resistance.
"Our study does not look at the currently licensed pneumococcal vaccines that are both safe and effective and reduce life threatening disease globally," said co-author Atkins. "Instead we looked at the impact of the new generation of pneumococcal vaccines," she said, noting "our results underscore the need for a highly effective [universal] vaccine because it would reduce the burden of both drug sensitive and drug resistant infections."
The analysis by Davies and colleagues arrives as the World Health Organization has stepped up its campaign dissuading the abuse, misuse and overuse of all antimicrobials, including antibiotics. Global antibiotic use increased 65% between 2000 and 2015, according to WHO, despite highly publicized efforts to halt unnecessary antibiotic prescriptions for humans and the use of antibiotics in feed products given to animals farmed for their meat.
WHO predicts drug resistance could kill more people worldwide than cancer by 2050 unless steps are taken now to reverse course on driving the global incidence of antimicrobial resistance. As it now stands, overexposure to the medications continues to give rise to untreatable superbugs. One solution, at least with respect to pneumococcal infections, some scientists say, is the development of vaccines that boost immunity against a wider variety of pneumococcal serotypes.
Currently, pneumococcal vaccines target only a portion of the known 100-plus pneumococcal serotypes. One commonly prescribed pneumococcal vaccine, PCV13, also known as Prevnar, targets 13 serotypes of Streptococcus pneumoniae: serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 19A, 19F, 18C, and 23F. The vaccine known as PPSV23 targets more—23 serotypes of the bacteria, including the 13 in Prevnar. There are, however, dozens of other pneumococcal serotypes for which there is no vaccine.
Davies, Atkins and colleagues contend that the "intersection of bacterial vaccines and antibiotic resistance needs more study." Their four mathematical models, for instance, capture potential patterns in antibiotic resistance. The models also reveal country-specific factors, such as differences in competition between drug-resistant and drug-sensitive bacteria. The scientists discovered that the type of pneumococcal vaccine deployed determined much of any given vaccine's impact on the evolution of antibiotic resistance. For example, the researchers predicted that universal, non-serotype-specific vaccines that accelerate clearance of bacteria may be better at preventing the spread of antibiotic resistant serotypes than vaccines that simply block acquisition of infection.
But while the British team examined patterns of drug resistance, other research groups have explored how vaccination saves money while preventing the emergence of drug resistant bacteria.
In the United States, scientists at North Carolina State University, and the University of North Carolina at Chapel Hill, found broad economic savings when vaccines are used to mitigate the development of antimicrobial resistance.
Focusing on pneumococcal infections in Ethiopia, Drs. Andrew Stringer and Sachiko Ozawa using their own mathematical model, found that vaccinating against pneumococcus helped slow the emergence of bacteria resistant to amoxicillin by nearly 15%. Vaccination slowed the emergence of bacteria resistant to ceftriaxone less significantly—only 0.59%—but the trend was in the right direction, findings showed.
Maintaining pneumococcal vaccination at the level identified in the model, the U.S. researchers estimated that would contribute an additional $7.67 million in annual savings for Ethiopia. Moreover, the money would not be lost to treating illnesses caused by drug-resistant pneumococcal infections.
"We wanted to model the value of vaccinating—not only to show that vaccination reduces death or disability from these diseases, but also to quantify whether vaccination can slow antimicrobial resistance," Stringer, an assistant professor of veterinary and global health at North Carolina State, said in a statement.
In the U.K., Davies and colleagues' four models capture potential patterns in antibiotic resistance. For example, vaccines with a high level of effectiveness are needed to reduce resistance in their model of a high-burden region where pneumococcal infections and antibiotic resistance are high. These findings "[highlight] that policies for managing antibiotic resistance with vaccines must be tailored to a specific pathogen and setting," the authors concluded.
Vaccination slows antimicrobial resistance
More information: Nicholas G. Davies et al, Modeling the effect of vaccination on selection for antibiotic resistance in Streptococcus pneumoniae, Science Translational Medicine (2021). DOI: 10.1126/scitranslmed.aaz8690
Journal information: Science Translational Medicine
© 2021 Science X Network
No comments:
Post a Comment