UPDATED

First woman reported cured of HIV after stem cell transplant
By Julie Steenhuysen - Yesterday
CHICAGO (Reuters) - A U.S. patient with leukemia has become the first woman and the third person to date to be cured of HIV after receiving a stem cell transplant from a donor who was naturally resistant to the virus that causes AIDS, researchers reported on Tuesday.
The case of a middle-aged woman of mixed race, presented at the Conference on Retroviruses and Opportunisitic Infections in Denver, is also the first involving umbilical cord blood, a newer approach that may make the treatment available to more people.
Since receiving the cord blood to treat her acute myeloid leukemia - a cancer that starts in blood-forming cells in the bone marrow - the woman has been in remission and free of the virus for 14 months, without the need for potent HIV treatments known as antiretroviral therapy.
The two prior cases occurred in males - one white and one Latino - who had received adult stem cells, which are more frequently used in bone marrow transplants.
"This is now the third report of a cure in this setting, and the first in a woman living with HIV," Sharon Lewin, President-Elect of the International AIDS Society, said in a statement.
The case is part of a larger U.S.-backed study led by Dr. Yvonne Bryson of the University of California Los Angeles (UCLA), and Dr. Deborah Persaud of Johns Hopkins University in Baltimore. It aims to follow 25 people with HIV who undergo a transplant with stem cells taken from umbilical cord blood for the treatment of cancer and other serious conditions.
Patients in the trial first undergo chemotherapy to kill off the cancerous immune cells. Doctors then transplant stem cells from individuals with a specific genetic mutation in which they lack receptors used by the virus to infect cells.
Scientists believe these individuals then develop an immune system resistant to HIV.
Lewin said bone marrow transplants are not a viable strategy to cure most people living with HIV. But the report "confirms that a cure for HIV is possible and further strengthens using gene therapy as a viable strategy for an HIV cure," she said.
The study suggests that an important element to the success is the transplantation of HIV-resistant cells. Previously, scientists believed that a common stem cell transplant side effect called graft-versus-host disease, in which the donor immune system attacks the recipient’s immune system, played a role in a possible cure.
"Taken together, these three cases of a cure post stem cell transplant all help in teasing out the various components of the transplant that were absolutely key to a cure," Lewin said.
(Reporting by Julie Steenhuysen; Editing by Bill Berkrot and David Gregorio)
Third person apparently cured of HIV using novel stem cell transplant
Patient is mixed-race woman treated in New York using umbilical cord blood, in technique raising chances of finding suitable donors
Patient is mixed-race woman treated in New York using umbilical cord blood, in technique raising chances of finding suitable donors
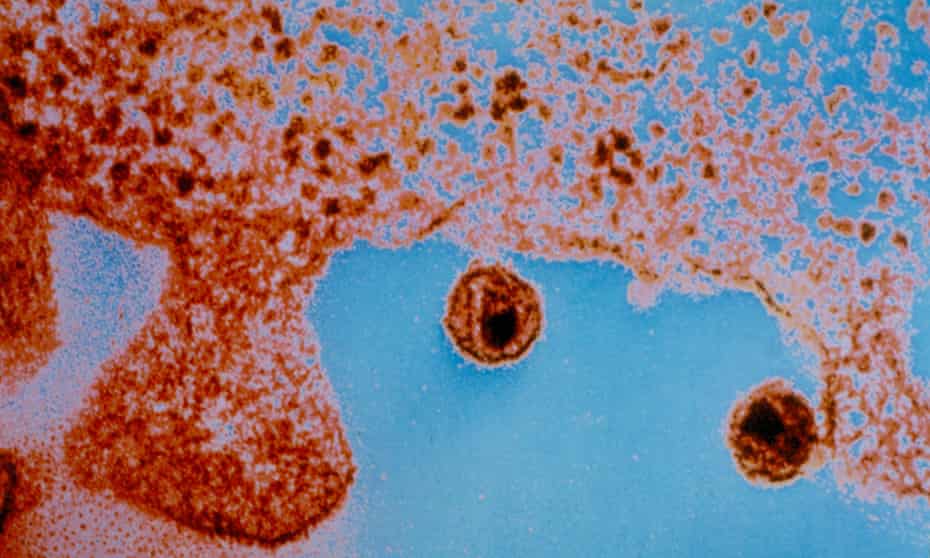
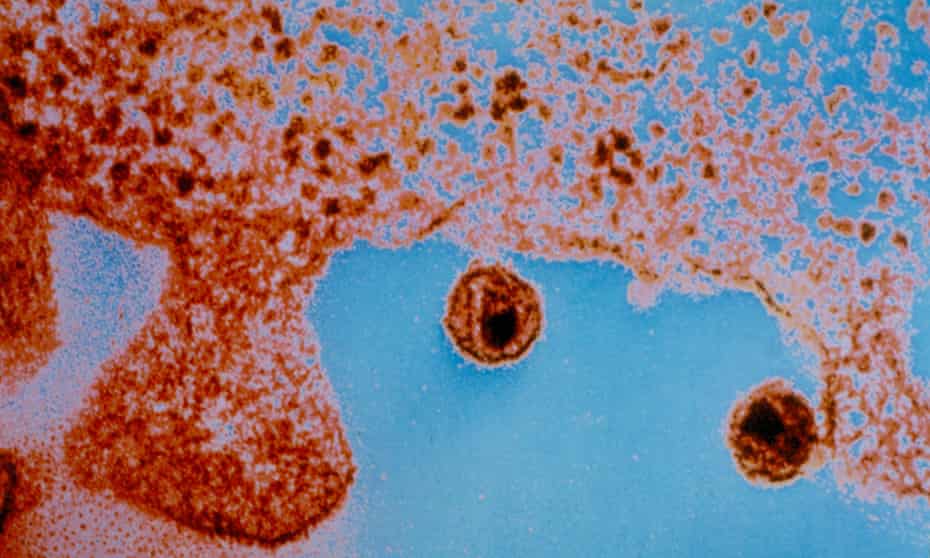
Doctor involved in the treatment estimates 50 people a year in the US could benefit. Photograph: Universal History Archive/Universal Images Group/Getty Images
Maya Yang
Maya Yang
THE GUARDIAN
Tue 15 Feb 2022
Scientists appear to have cured a third person, and the first woman, of HIV using a novel stem cell transplant method, American researchers in Denver, Colorado, said on Tuesday.
The patient, a woman of mixed race, was treated using a new method that involved umbilical cord blood, which is more readily available than the adult stem cells which are often used in bone marrow transplants, according to the New York Times.
Umbilical cord stem cells also do not need to be matched as closely to the recipient as bone marrow cells do.

HIV after Covid: Anthony Fauci and an army of researchers seek to regain momentum
“We estimate that there are approximately 50 patients per year in the US who could benefit from this procedure,” said Dr Koen van Besien, one of the doctors involved in the treatment.
“The ability to use partially matched umbilical cord blood grafts greatly increases the likelihood of finding suitable donors for such patients.”
The group of researchers revealed some of the case details at the Conference on Retroviruses and Opportunistic Infections in Denver. The woman is being called the “New York patient” by scientists, because she received the treatment at the New York-Presbyterian Weill Cornell Medical Center.
In 2013, she was diagnosed with HIV. Four years later, she was diagnosed with leukemia. In a procedure known as a haplo-cord transplant, she was given cord blood from a partially matched donor to treat her cancer. A close relative also provided her with blood to boost her immune system as she underwent the transplant.
After patients receive an umbilical cord blood transplant, they are then given additional adult stem cells. The stem cells grow quickly but are eventually replaced by cord blood cells.
Although cord blood is more adaptable than adult stem cells, it does not yield enough to serve as effective treatments of cancer in adults. As a result, in haplo-cord transplants, the additional transplant of stem cells helps make up for the scarcity of cord blood cells.
“The role of the adult donor cells is to hasten the early engraftment process and render the transplant easier and safer,” said Van Besien.
Since the woman’s transplant in August 2017, she has been in remission from her leukemia for more than four years. Three years after the transplant, she and her doctors discontinued her HIV treatment. Fourteen months since, she has yet to experience any resurgent virus.
According to the scientists, the majority of donors in registries are of Caucasian descent. As a result, allowing for only partial matches can open up the potential to treat patients who have both HIV and cancer, and also those who come from more diverse racial backgrounds.
“The fact that she’s mixed race, and that she’s a woman, that is really important scientifically and really important in terms of the community impact,” Dr Steven Deeks, an Aids expert at the University of California, told the Times.
Even though more than half of the world’s 35m HIV cases are found in women, women only make up 11% of participants in cure trials.
Although Deeks was not involved in the case, he acknowledged that “these are stories of providing inspiration to the field and perhaps the road map.
“Umbilical stem cells are attractive,” he added. “There’s something magical about these cells and something magical perhaps about the cord blood in general that provides an extra benefit.”
Tue 15 Feb 2022
Scientists appear to have cured a third person, and the first woman, of HIV using a novel stem cell transplant method, American researchers in Denver, Colorado, said on Tuesday.
The patient, a woman of mixed race, was treated using a new method that involved umbilical cord blood, which is more readily available than the adult stem cells which are often used in bone marrow transplants, according to the New York Times.
Umbilical cord stem cells also do not need to be matched as closely to the recipient as bone marrow cells do.

HIV after Covid: Anthony Fauci and an army of researchers seek to regain momentum
“We estimate that there are approximately 50 patients per year in the US who could benefit from this procedure,” said Dr Koen van Besien, one of the doctors involved in the treatment.
“The ability to use partially matched umbilical cord blood grafts greatly increases the likelihood of finding suitable donors for such patients.”
The group of researchers revealed some of the case details at the Conference on Retroviruses and Opportunistic Infections in Denver. The woman is being called the “New York patient” by scientists, because she received the treatment at the New York-Presbyterian Weill Cornell Medical Center.
In 2013, she was diagnosed with HIV. Four years later, she was diagnosed with leukemia. In a procedure known as a haplo-cord transplant, she was given cord blood from a partially matched donor to treat her cancer. A close relative also provided her with blood to boost her immune system as she underwent the transplant.
After patients receive an umbilical cord blood transplant, they are then given additional adult stem cells. The stem cells grow quickly but are eventually replaced by cord blood cells.
Although cord blood is more adaptable than adult stem cells, it does not yield enough to serve as effective treatments of cancer in adults. As a result, in haplo-cord transplants, the additional transplant of stem cells helps make up for the scarcity of cord blood cells.
“The role of the adult donor cells is to hasten the early engraftment process and render the transplant easier and safer,” said Van Besien.
Since the woman’s transplant in August 2017, she has been in remission from her leukemia for more than four years. Three years after the transplant, she and her doctors discontinued her HIV treatment. Fourteen months since, she has yet to experience any resurgent virus.
According to the scientists, the majority of donors in registries are of Caucasian descent. As a result, allowing for only partial matches can open up the potential to treat patients who have both HIV and cancer, and also those who come from more diverse racial backgrounds.
“The fact that she’s mixed race, and that she’s a woman, that is really important scientifically and really important in terms of the community impact,” Dr Steven Deeks, an Aids expert at the University of California, told the Times.
Even though more than half of the world’s 35m HIV cases are found in women, women only make up 11% of participants in cure trials.
Although Deeks was not involved in the case, he acknowledged that “these are stories of providing inspiration to the field and perhaps the road map.
“Umbilical stem cells are attractive,” he added. “There’s something magical about these cells and something magical perhaps about the cord blood in general that provides an extra benefit.”
Woman Cured of HIV Using New Method Shows Potential for Others: Scientists
BY LORA KORPAR ON 2/15/22
A stem cell transplant has appeared to cure the human immunodeficiency virus (HIV) in a woman for the first time.
This is the third known case of HIV remission from a stem cell transplant, the National Institute of Allergy and Infectious Diseases (NIAID) said in a news release. It's a massive breakthrough in treatment for a virus that for decades was completely incurable.
The woman, who has not yet been named, joins two men who have been cured or likely been cured of the virus, NBC News reported. However, there is still a ways to go before the treatment can be widely used. It's a risky procedure involving the destruction of the immune system, so scientists have only tried it on those suffering from potentially deadly cancers. The patient had received the stem cell transplant to treat her acute myeloid leukemia, according to the NIAID.
The new treatment uses stem cells from umbilical cord blood, which are more widely available than adult stem cells, The New York Times reported. There has been no detected HIV in the woman for 14 months, the NIAID release said, even after stopping antiretroviral therapy, an HIV treatment.

A woman has likely been cured of HIV for the first time.
Above, a woman is seen holding an HIV/AIDS awareness ribbon.
STOCK IMAGE/GETTY IMAGES
The treatment works by essentially destroying one's immune system and replacing it with a new one, which treats the person's cancer while curing their HIV.
"By killing off the cancerous immune cells via chemotherapy and then transplanting stem cells with the CCR5 genetic mutation, scientists theorize that people with HIV then develop an HIV-resistant immune system," the NIAID said.
Experts told NBC News that this treatment would be "unethical" if tried on someone without life-threatening cancer or another medical condition that qualifies them for it, as it is "toxic" and "sometimes fatal."
Dr. Deborah Persaud, a pediatric infectious disease specialist and one of the leaders of the study, told the outlet while the stem cell transplant is an exciting development, it is "still not a feasible strategy for all but a handful of the millions of people living with HIV."
The first man cured using the stem cell treatment, known as the "Berlin patient," was in HIV remission for 12 years and deemed cured of it before his death from leukemia in September 2020, according to the NIAID. The second man, dubbed the "London patient," continues to be in remission after 30 months.
The treatment works by essentially destroying one's immune system and replacing it with a new one, which treats the person's cancer while curing their HIV.
"By killing off the cancerous immune cells via chemotherapy and then transplanting stem cells with the CCR5 genetic mutation, scientists theorize that people with HIV then develop an HIV-resistant immune system," the NIAID said.
Experts told NBC News that this treatment would be "unethical" if tried on someone without life-threatening cancer or another medical condition that qualifies them for it, as it is "toxic" and "sometimes fatal."
Dr. Deborah Persaud, a pediatric infectious disease specialist and one of the leaders of the study, told the outlet while the stem cell transplant is an exciting development, it is "still not a feasible strategy for all but a handful of the millions of people living with HIV."
The first man cured using the stem cell treatment, known as the "Berlin patient," was in HIV remission for 12 years and deemed cured of it before his death from leukemia in September 2020, according to the NIAID. The second man, dubbed the "London patient," continues to be in remission after 30 months.
HIV attacks the immune system and, if not treated, can lead to AIDS, which makes one susceptible to many severe illnesses, called "opportunistic infections," according to the U.S. Centers for Disease Control and Prevention (CDC). While cases of HIV and AIDS have declined since peaks in the 1980s and 1990s, the Kaiser Family Foundation reported as of June 2021, there were 1.2 million people living with HIV in the United States.
Remedy Deemed Too Risky for Healthy Patients After First Woman Cured of HIV
Justin Klawans - Yesterday
Newsweek
While a risky stem cell therapy has successfully cured the first woman of the human immunodeficiency virus (HIV), the procedure is deemed too dangerous to use on the average patient.

© iStock/Getty
An experimental stem cell treatment has successfully cured a woman of HIV. However, the procedure is considered extremely risky and potentially dangerous, and as a result it is only being offered to HIV patients with end-stage cancer. Here, stem cells from human bone marrow can be seen under a microscope.
The therapy—known as a cord blood stem cell transplant—was given to an American woman from a donor who was naturally immune to HIV, according to a press release issued Tuesday from the National Institute of Allergy and Infectious Diseases (NIAID). She became the third person overall and first woman to be declared cured of HIV after the virus was not detected in her system within 14 months.
The case is also reportedly the first involving the use of umbilical cord blood, a newer approach could provide further breakthroughs.
However, despite the woman appearing to have been cured, researchers have reiterated that the therapy is still considered extremely risky and has only been tested on patients suffering from end-stage cancers, such as the woman—who had been diagnosed with acute myeloid leukemia. Experts told NBC News that it would even be considered "unethical" to attempt the transplant in an otherwise healthy patient due to its danger.
The risk comes, scientists stated, because of the nature of the transplanted bone marrow, which attacks a patient's cancerous immune system in an effort to replace it with one containing the HIV-immune cells of the donor. This, in theory, means that the patient's immune system is being completely replaced by another person's, which both treats the cancer and cures them of HIV.
"By killing off the cancerous immune cells via chemotherapy and then transplanting stem cells with the CCR5 genetic mutation, scientists theorize that people with HIV then develop an HIV-resistant immune system," NIAID said.
However, the complex procedure can often result in the death of the patient, scientists told NBC News, and as a result the treatment is not offered for those who do not already have a potentially fatal illness.
"[The stem cell treatment is] still not a feasible strategy for all but a handful of the millions of people living with HIV," Dr. Deborah Persaud, a pediatric infectious disease specialist at Johns Hopkins University and one of the chairs of the case study, stated. However, Persaud added that, despite this, her team was still "very excited" about the potential future of the treatment.
Additionally, Sharon Lewin, the president-elect of the International AIDS Society, expressed hope that the three combined cases could eventually be used to develop a stem cell therapy that is safe for the masses.
"Taken together, these three cases of a cure post stem cell transplant all help in teasing out the various components of the transplant that were absolutely key to a cure," Lewin said in a statement.
HIV and its associated illness, acquired immunodeficiency syndrome (AIDS), are most often treated using a combination of drugs and experimental tests, as in the three people who have been cured therapeutically. However, there have been extremely rare cases of an HIV-positive person being "naturally" cured of the virus.
In November 2021, a woman in Argentina became the second documented HIV patient whose own immune system cured her of the disease, with no outside intervention.
"This is really the miracle of the human immune system that did it," Dr. Xu Yu, one of the leaders of the Argentine case study, said at the time.
Newsweek has contacted the CDC's National Center for HIV, Hepatitis, STD and TB Prevention for comment.
The therapy—known as a cord blood stem cell transplant—was given to an American woman from a donor who was naturally immune to HIV, according to a press release issued Tuesday from the National Institute of Allergy and Infectious Diseases (NIAID). She became the third person overall and first woman to be declared cured of HIV after the virus was not detected in her system within 14 months.
The case is also reportedly the first involving the use of umbilical cord blood, a newer approach could provide further breakthroughs.
However, despite the woman appearing to have been cured, researchers have reiterated that the therapy is still considered extremely risky and has only been tested on patients suffering from end-stage cancers, such as the woman—who had been diagnosed with acute myeloid leukemia. Experts told NBC News that it would even be considered "unethical" to attempt the transplant in an otherwise healthy patient due to its danger.
The risk comes, scientists stated, because of the nature of the transplanted bone marrow, which attacks a patient's cancerous immune system in an effort to replace it with one containing the HIV-immune cells of the donor. This, in theory, means that the patient's immune system is being completely replaced by another person's, which both treats the cancer and cures them of HIV.
"By killing off the cancerous immune cells via chemotherapy and then transplanting stem cells with the CCR5 genetic mutation, scientists theorize that people with HIV then develop an HIV-resistant immune system," NIAID said.
However, the complex procedure can often result in the death of the patient, scientists told NBC News, and as a result the treatment is not offered for those who do not already have a potentially fatal illness.
"[The stem cell treatment is] still not a feasible strategy for all but a handful of the millions of people living with HIV," Dr. Deborah Persaud, a pediatric infectious disease specialist at Johns Hopkins University and one of the chairs of the case study, stated. However, Persaud added that, despite this, her team was still "very excited" about the potential future of the treatment.
Additionally, Sharon Lewin, the president-elect of the International AIDS Society, expressed hope that the three combined cases could eventually be used to develop a stem cell therapy that is safe for the masses.
"Taken together, these three cases of a cure post stem cell transplant all help in teasing out the various components of the transplant that were absolutely key to a cure," Lewin said in a statement.
HIV and its associated illness, acquired immunodeficiency syndrome (AIDS), are most often treated using a combination of drugs and experimental tests, as in the three people who have been cured therapeutically. However, there have been extremely rare cases of an HIV-positive person being "naturally" cured of the virus.
In November 2021, a woman in Argentina became the second documented HIV patient whose own immune system cured her of the disease, with no outside intervention.
"This is really the miracle of the human immune system that did it," Dr. Xu Yu, one of the leaders of the Argentine case study, said at the time.
Newsweek has contacted the CDC's National Center for HIV, Hepatitis, STD and TB Prevention for comment.
No comments:
Post a Comment