LATAM airline to lay off 2,700 crew

AUGUST 1, 2020
Latin America's biggest airline, the Brazilian-Chilean group LATAM, said Friday it was laying off at least 2,700 crew to cope with the devastating effects of the coronavirus pandemic on the aviation industry.
LATAM said it had failed to reach a deal with the aviation workers' union on reducing pay, and would therefore lay off pilots and flight attendants to keep the struggling company afloat.
The layoffs amount to more than a third of the airline's total crew.
"The COVID-19 pandemic is the biggest public health crisis in history, and is dramatically affecting the entire world aviation industry," the company said in a statement.
It will offer a voluntary departure plan until Tuesday, then begin laying people off if necessary, it said.
It said crew pay at LATAM was above average for the region, and that "the current crisis has made it more essential than ever" to reduce its wage bill.
The airline filed for bankruptcy in the United States in May, after worldwide stay-at-home measures to contain the virus forced it to reduce its operations by 95 percent.
Explore further Latin America's largest airline LATAM files for bankruptcy in US
jULY 31, 2020
Spirit Airlines warns of layoffs, ExpressJet's fate in doubt
Spirit Airlines has warned up to 30% of its employees that they will lose their jobs in October, and regional carrier ExpressJet's future is in doubt after losing a key contract as the virus pandemic continues to hammer the airline industry.
Spirit is the latest airline to deliver layoff warnings to employees, which are required by federal law 60 days before large-scale job cuts.
The budget airline based in Miramar, Florida, said it told unions that about 20% to 30% of its pilots, flight attendants and other groups will be furloughed in October. The airline did not give a number. It had 9,100 employees at the start of the year. Spirit said it hopes to restore the jobs eventually.
Earlier in July, United Airlines issued layoff warnings for 36,000 employees, and it warned pilots this week of possible additional job losses this year and next year. American Airlines notified 25,000 workers that they could be furloughed in October, when billions in federal money to help cover payroll costs expires.
Airlines are slashing costs, getting federal aid and borrowing on private credit markets to survive a downturn in U.S. air travel that hit 95% in April. Hopes for a recovery have dimmed in recent weeks with a resurgence of reported cases of COVID-19 in many states, which ended two months of growth in air travel.
The retrenchment now threatens another small U.S. airline. ExpressJet's survival was in doubt after United dropped its contract with ExpressJet and consolidated its United Express operations under affiliate CommutAir. United spokesman Charles Hobart said the change will take a "number of months."
ExpressJet spokesman Gary Cambre said the airline expects to continue normal operations through the rest of this year. "We will now explore all options for the future of our company in 2021," he said in an emailed statement.
The Regional Airline Association, of which ExpressJet is a member, said the Atlanta-based carrier's announcement "reflects the double-edged sword regional airlines encounter as they navigate the pandemic"—the virus is harming their companies and the major airlines they serve under contracts.
The trade group is lobbying for an extension of the federal aid to help airlines cover their payroll costs, which runs out in October.
"For ExpressJet, it may already be too late," the group said.
Earlier this year, Trans States and Compass airlines shut down after major airline partners reduced regional flights due to the pandemic. Alaska's Ravn Air also stopped flying.
© 2020 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.
Air Canada takes huge loss amid pandemic travel shutdown

Air Canada on Friday announced a loss of more than CAN$1.7 billion (US$1.27 billion) in the second quarter due to the "devastating effects" of the coronavirus pandemic.
With travel at a near standstill, the airline's revenue fell 89 percent in the April-June period, with most flights suspended due to containment measures and border closings imposed to stem the pandemic, Air Canada said in a statement.
The number of passengers fell 96 percent compared to a year ago, forcing Air Canada to cut 20,000 jobs, more than half its workforce, the company said.
"As with many other major airlines worldwide, Air Canada's second quarter results confirm the devastating and unprecedented effects of the COVID-19 pandemic," the airline's chief Calin Rovinescu said.
Revenue plummeted to $527 million, compared to over $4.7 billion in the same period in 2019, when the airline saw net income of $343 million.
In contrast with the shutdown of passenger service, cargo revenue rose 52 percent to $269 million, with the conversion of Boeing 777s and 787s to carry medical equipment to deal with the pandemic.
Citing a "impossible operating environment" after Canada imposed some of the world's "most severe" restrictions, Rovinescu called on Ottawa "to take prudent steps to replace current blanket travel restrictions and quarantines with targeted evidence-based measures that reflect current circumstances."
After taking some painful steps to respond to the unprecedented crisis, he said the airline is looking forward to the "equally unprecedented opportunity to rebuild a smaller but even more nimble airline, with a simplified and younger fleet and a lower cost structure coming out of the crisis."
© 2020 AFP
























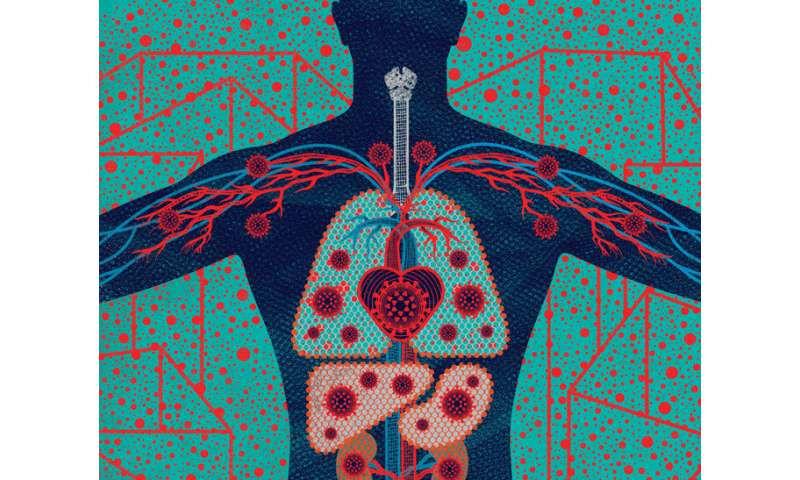

 From Head to “COVID Toes”: People with COVID-19 exhibit from none to many of these symptoms. Some symptoms (such as fever, cough, and loss of smell) are common, while others (such as sore throat, pink eye, and stroke) are rare. Credit: Illustration: Stephanie Koch. Concept: Jennifer Babik, M.D., Ph.D.
From Head to “COVID Toes”: People with COVID-19 exhibit from none to many of these symptoms. Some symptoms (such as fever, cough, and loss of smell) are common, while others (such as sore throat, pink eye, and stroke) are rare. Credit: Illustration: Stephanie Koch. Concept: Jennifer Babik, M.D., Ph.D.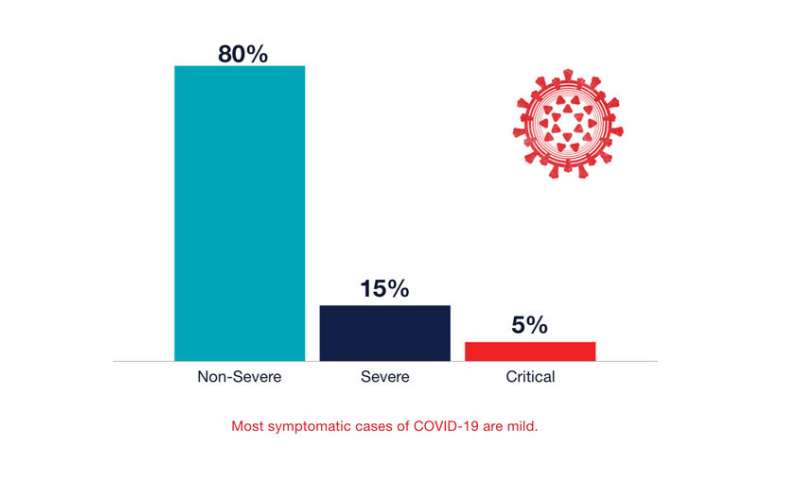 Most symptomatic cases of COVID-19 are mild. Credit: UCSF
Most symptomatic cases of COVID-19 are mild. Credit: UCSF