Massachusetts
Fueling St. Vincent strike: Pandemic, nursing shortage, opinions about corporate health
Cyrus Moulton
Telegram & Gazette

WORCESTER — Aimee Albani said nursing has changed a lot in her 43 years in the field.
She has been kicked, spat on and had to call for help as more and more patients go through withdrawal from alcohol and drugs.
She has dealt with increasing numbers of “armchair physicians” who insist they know how to better do her job and an increasingly litigious society.
And she has witnessed staffing shortages as the gray tsunami crests, experienced corporate cost-cutting, and watched colleagues leave for hospitals with better pay and benefits.
It made Albani consider quitting.
Then came COVID-19.
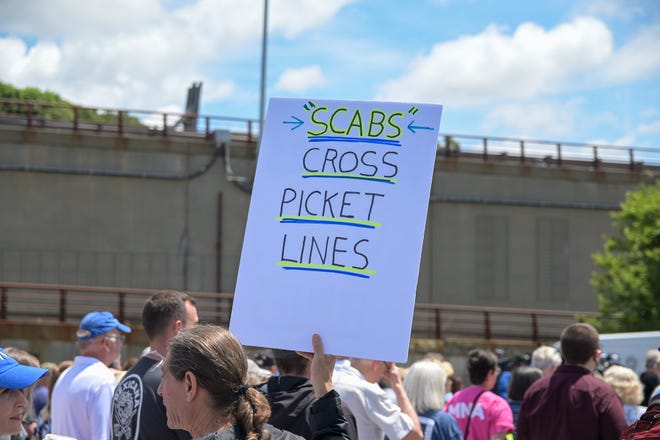
“I was going to quit if staffing didn’t improve, but then I wasn’t going to quit during COVID, I didn’t want to leave my colleagues,” Albani said Wednesday while on the picket line outside St. Vincent Hospital.
But “COVID was awful,” Albani continued. “(It) just made it worse.”
While the daily back and forth between St. Vincent Hospital leaders and Massachusetts Nurses Association focus on audit committees, other hospitals’ staffing language, resource nurses and whether the offers were insulting, not serious or “opened the door to substantive discussions,” it can be difficult to take a step back and try and put the strike in a larger context.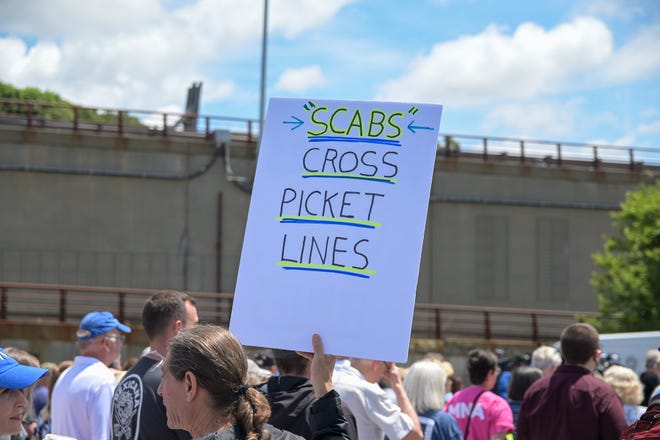
Why is the strike happening?
For instance, why is this strike happening here and now? Why has it gone on so long and drawn even nationalattention? And while both sides agree staffing is the main issue in the strike, can the debate over whether 1-to-5 versus 1-to-4 staffing ratios are appropriate on different units be separated from larger issues?
Those questions are difficult to definitively answer.
But discussions since the beginning of the strike with nurses, union officials, St. Vincent leaders and experts on labor help put the strike in some context.
“I definitely think there are other larger issues,” Carolyn Jackson, CEO of St. Vincent Hospital, said in an interview Thursday. “I think there has been a lot going on in health care with the pandemic and many things across the country and locally.”
David Schildmeier, a spokesman for the MNA, agreed.
“This is a broader issue, that’s why the nurses strike has struck such a chord across the country,” Schildmeier said.
Those interviewed generally focused on three factors that have played a role in the nurses’ strike: the COVID pandemic, a nursing shortage, and feelings about the corporatization of health care.
None of these factors are independent. Multiple people interviewed said COVID made the nursing shortage more acute, for instance.
Much of the evidence is also primarily anecdotal. For instance, effects of COVID may not be known for many years, and numbers and data concerning the pandemic are still being collected as the virus remains with us.
“Certainly (the nurses) tell us they have to take on too many patients,” Hans Despain, a professor of economics at Nichols College who has been following the strike, said. “What’s more difficult is finding the actual data…But I trust the chorus of nurses saying this is a reflection of the trend.”
Data on strikes are similarly limited: The Bureau of Labor Statistics only tracks strikes involving 1,000 or more workers, so the strike at St. Vincent doesn’t even register.
But the entire world experienced the pandemic.
A strike is happening here.
“As I say, it wasn’t in New York or Los Angeles, it was in Worcester, Mass.,” said Tom Juravich, a professor in the Labor Center at the University of Massachusetts at Amherst and a union consultant. “That the nurses stood up to Tenet (the company that owns St. Vincent Hospital), I think there’s a lot of symbols here.”
COVID pandemic and nursing
The biggest issue that pretty much all of those interviewed identified when asked what has affected the strike was no surprise: the COVID pandemic.
“Some of what has gone across the country with picketing and some things really has to do with the stress of the pandemic,” Jackson said. “It put a strain on the overall health care workforce.”
The city confirmed its first COVID case on March 14, 2020, culminating a week when the virus became a national emergency, Gov. Charlie Baker declared a state of emergency, schools and other public facilities closed, and the state shut down.
Health care workers were on the front line and among those rightly praised as heroes, receiving tributes ranging from a fighter jet flyover to tree plantings to parades.
The support was welcome. Hospital workers experienced a lot, including burnout and depression and anxiety as they dealt with a virus that was so new that guidance on treating it often changed by the day.
Now, clearly a once-in-a-lifetime pandemic in a country with a health care system as complex — and, according to many, broken — as ours would tax many hospitals.
But several St. Vincent nurses felt the situation at the hospital was particularly bad.
“When it first came, we were totally unprepared,” Albani said. “It was like they didn’t take the fact that it was coming seriously ... I really didn’t feel at all supported by the hospital.”
Nurse Marie Ritacco, a member of the union’s bargaining committee at the hospital, agreed.
“It got exponentially worse when the middle of March last year came,” she said.
PPE complaints
Several nurses complained that PPE was not readily available; even “hidden” or “locked up,” according to Albani.
St. Vincent leaders disputed this characterization.
“During this time, the hospital never ran out of personal protective equipment, continuously implemented rigorous COVID SAFETY standards and increased access to vaccinations,” a March 2, 2021 letter from the St. Vincent Hospital Board of Trustees read.
Jackson concurred. She said the hospital “never ran out of PPE” and, in fact, had 11,000 rain ponchos that it never had to deploy for use. She also said the hospital had “minimum” staff-to-staff and patient-to-staff infections compared to some peer institutions.
“Everybody had challenges, but I would say that we did better than a lot of the hospitals that I have talked to in the state and across the country,” Jackson said. “Having adequate PPE, having tight at times but appropriate staffing, and minimal staff infections, we did pretty well.”
Nurses nevertheless put in long hours in a physically and mentally demanding situation, often with highly acute patients.
And in the midst of COVID - and a day after nurses unanimously rejected a proposed contract and also after the state announced almost $1 billion to shore up the health care industry in response to COVID, St. Vincent Hospital announced furloughs.
The hospital said the furloughs were voluntary and that more workers applied than were required. Nurses disagreed with this characterization.
But coming amidst contract disputes and in the midst of a health care crisis, nurses said they felt betrayed.
“The pandemic just made us realize that things were only going to get worse for us if we didn’t take a stand now,” Ritacco said. “Employers like ours looked at what we were able to do during the pandemic and decided that that would become our new norm, and we knew we could not perform at those crises level without really harming people in the process, and we were not going to accept that going forward...That experience just solidified for us that they were not to be trusted.”
Outside observers agree about the impact of COVID.
“I think (COVID) is really what pushed the St. Vincent’s issue to a head,” said Despain. “They already had the main dispute of staffing, then the hours put in by nurses went up because of COVID, and they just couldn’t come to an agreement.”
Juravich said the COVID “crisis” has put “all kinds of pressures on the health care industry.”
“There’s been a great need for health care because of COVID, but it’s also got in the way of hospitals doing elective surgeries, which is where they make profits,” Juravich said. “We’ve also seen a lot of activism and militarism from nurses and advocacy.”
“I think that we’ve seen across the country, nurses, and people in health care standing up and saying we deserve to be treated well,” Juravich continued. “I think that’s playing out in Worcester. Nurse-to-patient ratios do matter, and they matter a lot to their ability to do good work.”
Monica Carney, a professor of economics at the College of the Holy Cross who specializes in health care and labor, agreed that staffing ratios matter.
“I think that it’s become more apparent that support and staffing ratios matter in health care, particularly that’s important because of the pandemic,” Carney said in an interview.
Nursing shortage
But nurse-to-patient ratios are hard to fill when there is a shortage of nurses.
“Right now is a wonderful time to be entering the nursing workforce: I believe it’s a buyer’s market for nurses,” Pat Creelman, a professor of nurse education at Quinsigamond Community College, said. “Many facilities are offering sign-on bonuses because the number of nurses is so low, even for new graduates...the jobs are plentiful.”
Ethan Roden, director of human resources and operations for MSG Staffing in Worcester, agreed.
“Nurses have their pick in this present market,” Roden said in an email. “Everyone is sourcing the same candidates for the same positions. Nurses have the ability to choose where they would like to work and at what price. Nurses will not settle for less.”
According to the Bureau of Labor Statistics’ Occupational Outlook Handbook, employment of registered nurses is projected to grow 7% from 2019 to 2029, “faster than the average for all occupations.”
“Growth will occur for a number of reasons, including an increased emphasis on preventive care; increasing rates of chronic conditions, such as diabetes and obesity; and demand for health care services from the baby-boom population, as this group leads longer and more active lives,” according to the BLS.
The extent of the local shortage is difficult to determine, however.
According to a Department of Public Health spokesperson, the executive director of the state’s Board of Registration in Nursing said “she didn’t have any information or data that would be useful to share for your story.” Two queries for an interview with a representative of the Massachusetts Health and Hospital Association for this story yielded no results. Moreover, Creelman said she “can’t really comment on St. Vincent’s and don’t want to.”
However, Creelman said that in 20 years at QCC, the ebb and flow of nurses is at a low.
“Probably, we’re in a better place than we were in 2005-2006. However, I’m finding those conversations starting up again in facilities about needing to find creative ways to attract staff,” Creelman said.
COVID also didn’t help the staffing shortage on the other end.
“I believe COVID has had a negative effect on nursing, in that a lot of people have chosen to retire because of the COVID pandemic, so that has also led to the shortage in nursing,” Creelman said.
Jackson said the workforce experienced both many workers deciding to retire early and workers taking leave because the lockdown gave them additional responsibilities at home.
Juravich also said nurses’ complaints about unsafe staffing and difficult working conditions didn’t help the shortage.
“One of the bigger issues is not how many people are coming into the pipeline but how many are leaving because of these types of working conditions,” Juravich said.
“If companies want to retain nurses, then they have to hold up the conditions and staffing that make it possible to be working,” Juravich continued. “There’s not a reserve army out there in Central Mass. or anywhere in the country of nurses who are willing to go anywhere and work for any company.”
Corporate ownership
Particularly a company where a lack of trust, and as Ritacco said earlier, exists between nurses and leadership. The nurses took a vote of no confidence in Jackson’s leadership in May 2020, and the trust has only further eroded since the beginning of the strike as the hospital’s spending on police details and travel nurses has nurses questioning the hospital’s priorities.
“With all the money wasted, they could have given it to the community, given it back to the hospital and hired the nurses we need,” Nurse Chris Cuthbert said Wednesday, citing an MNA estimate that Tenet has spent more than $75 million on the strike. Jackson has disputed MNA estimates as too high but not cited an exact cost of the strike.
“Tenet could have been a hero,” Cuthbert said. “Instead they’re a zero.”
Then there is the fact that this is the second go-around between the company and striking St. Vincent nurses.
It’s also pretty easy to criticize Tenet - a for-profit health care company with 65 hospitals and approximately 450 outpatient centers and “additional sites of care” that has paid $1.7 billion in penalties since 2000, according to Good Jobs First, a national policy resource center.
Again, the pandemic exacerbated the criticism.
“The apparent greed of Tenet Healthcare during an unprecedented public health emergency and economic crisis is astounding, particularly in light of the billions in taxpayer assistance received by your company, and the ongoing failure to address the concerns of its frontline health care workers,” U.S. Sens. Elizabeth Warren and Ed Markey and U.S. Reps. James P. McGovern and Lori Trahan wrote in a June 29 letter to Tenet’s CEO Ronald A. Rittenmeyer.
The letter noted that Tenet sought more than $2 billion in loans and grants from the federal government, “an effort you admitted was aimed at “maximizing [Tenet’s] cash position.” Moreover, despite the pandemic, Tenet reported annual earnings over $3.1 billion in 2020, and their stock price has increased fivefold from March 20, 2020, to June 16, 2021, according to the letter. The chain also produced a $97 million profit in the first quarter of 2021. Meanwhile, from April to June 2020, Tenet "slashed hospital spending by 11% or $377 million, while receiving more than $850 million of federal stimulus money," the letter said, citing a Tenet earnings release.
“Symbolically right now, and far beyond Worcester and the lines of the commonwealth, there is a sense that these larger corporations are sometimes not in the best interest of nurses and patients,” Juravich said. “I don’t know there is a lot of love for Tenet in Worcester.”
Juravich said that this corporate structure can lead to a disconnect between the goals of a for-profit company and the goals of nurses at the bedside.
“St. Vincent, like much of health care, has seen lots of buyouts and takeovers of smaller community hospitals, and it’s all well and good that you may want to run the hospital this way but we have traditions and practices, and our patients have needs that we need to fill on a local basis,” Juravich said. “Sometimes health care is not part of a larger strategic plan, sometimes it depends on what happens on the floors.”
Despain said this disconnect between corporate and local management is “a big part of the tension here.”
“You have a number of nurses who fundamentally don’t agree with the type of management put over them by Tenet,” Despain said. “Tenet meanwhile is trying to provide a profitable business and provide care. I don’t think Tenet is trying to not provide care; but when you do it on a shoestring, it becomes very precarious.”
Nurses concur, repeatedly referring over the course of the strike to St. Vincent Hospital as a Worcester - not a Tenet - institution.
“This is our community hospital,” nurse Dominique Muldoon said in an interview earlier this month.
Community members and politicians have also rallied to the nurses’ cause. As Schildmeier pointed out, nobody has been holding vigils or displaying lawn signs for Tenet.
But is it perhaps too easy to paint Tenet as the big, bad corporate Goliath?
“I prefer to call it a taxpaying hospital rather than a for-profit hospital,” Jackson continued. “We are quite important to the Worcester economy, not just for jobs we provide, but the tax revenue we provide for the city and the quality care we provide for the community.”
Jackson noted that the hospital was the third-largest taxpayer in the city, paying at least $13 million annually to city coffers.
“We provide excellent care and at a reasonable cost and I think Tenet has been a good steward of its hospital,” Jackson said.
The question is whether Tenet has been a good steward of its nurses.
Albani, back at the strike, didn’t think so.
She said that since Tenet took over at the hospital in 2013 the amount of supplies has decreased, there have been cheaper supplies, positions have been cut, vacant positions have not been filled soon enough, and staffing guidelines haven't been followed.
“This strike could be settled: The nurses that have been out here picketing are the hospital’s best asset as far as loyalty, integrity and commitment to patient safety,” Albani said. “They had the money, and they blew it.”
Cyrus Moulton
Telegram & Gazette
WORCESTER — Aimee Albani said nursing has changed a lot in her 43 years in the field.
She has been kicked, spat on and had to call for help as more and more patients go through withdrawal from alcohol and drugs.
She has dealt with increasing numbers of “armchair physicians” who insist they know how to better do her job and an increasingly litigious society.
And she has witnessed staffing shortages as the gray tsunami crests, experienced corporate cost-cutting, and watched colleagues leave for hospitals with better pay and benefits.
It made Albani consider quitting.
Then came COVID-19.
“I was going to quit if staffing didn’t improve, but then I wasn’t going to quit during COVID, I didn’t want to leave my colleagues,” Albani said Wednesday while on the picket line outside St. Vincent Hospital.
But “COVID was awful,” Albani continued. “(It) just made it worse.”
While the daily back and forth between St. Vincent Hospital leaders and Massachusetts Nurses Association focus on audit committees, other hospitals’ staffing language, resource nurses and whether the offers were insulting, not serious or “opened the door to substantive discussions,” it can be difficult to take a step back and try and put the strike in a larger context.
Why is the strike happening?
For instance, why is this strike happening here and now? Why has it gone on so long and drawn even nationalattention? And while both sides agree staffing is the main issue in the strike, can the debate over whether 1-to-5 versus 1-to-4 staffing ratios are appropriate on different units be separated from larger issues?
Those questions are difficult to definitively answer.
But discussions since the beginning of the strike with nurses, union officials, St. Vincent leaders and experts on labor help put the strike in some context.
“I definitely think there are other larger issues,” Carolyn Jackson, CEO of St. Vincent Hospital, said in an interview Thursday. “I think there has been a lot going on in health care with the pandemic and many things across the country and locally.”
David Schildmeier, a spokesman for the MNA, agreed.
“This is a broader issue, that’s why the nurses strike has struck such a chord across the country,” Schildmeier said.
Those interviewed generally focused on three factors that have played a role in the nurses’ strike: the COVID pandemic, a nursing shortage, and feelings about the corporatization of health care.
None of these factors are independent. Multiple people interviewed said COVID made the nursing shortage more acute, for instance.
Much of the evidence is also primarily anecdotal. For instance, effects of COVID may not be known for many years, and numbers and data concerning the pandemic are still being collected as the virus remains with us.
“Certainly (the nurses) tell us they have to take on too many patients,” Hans Despain, a professor of economics at Nichols College who has been following the strike, said. “What’s more difficult is finding the actual data…But I trust the chorus of nurses saying this is a reflection of the trend.”
Data on strikes are similarly limited: The Bureau of Labor Statistics only tracks strikes involving 1,000 or more workers, so the strike at St. Vincent doesn’t even register.
But the entire world experienced the pandemic.
A strike is happening here.
“As I say, it wasn’t in New York or Los Angeles, it was in Worcester, Mass.,” said Tom Juravich, a professor in the Labor Center at the University of Massachusetts at Amherst and a union consultant. “That the nurses stood up to Tenet (the company that owns St. Vincent Hospital), I think there’s a lot of symbols here.”

COVID pandemic and nursing
The biggest issue that pretty much all of those interviewed identified when asked what has affected the strike was no surprise: the COVID pandemic.
“Some of what has gone across the country with picketing and some things really has to do with the stress of the pandemic,” Jackson said. “It put a strain on the overall health care workforce.”
The city confirmed its first COVID case on March 14, 2020, culminating a week when the virus became a national emergency, Gov. Charlie Baker declared a state of emergency, schools and other public facilities closed, and the state shut down.
Health care workers were on the front line and among those rightly praised as heroes, receiving tributes ranging from a fighter jet flyover to tree plantings to parades.
The support was welcome. Hospital workers experienced a lot, including burnout and depression and anxiety as they dealt with a virus that was so new that guidance on treating it often changed by the day.
Now, clearly a once-in-a-lifetime pandemic in a country with a health care system as complex — and, according to many, broken — as ours would tax many hospitals.
But several St. Vincent nurses felt the situation at the hospital was particularly bad.
“When it first came, we were totally unprepared,” Albani said. “It was like they didn’t take the fact that it was coming seriously ... I really didn’t feel at all supported by the hospital.”
Nurse Marie Ritacco, a member of the union’s bargaining committee at the hospital, agreed.
“It got exponentially worse when the middle of March last year came,” she said.

PPE complaints
Several nurses complained that PPE was not readily available; even “hidden” or “locked up,” according to Albani.
St. Vincent leaders disputed this characterization.
“During this time, the hospital never ran out of personal protective equipment, continuously implemented rigorous COVID SAFETY standards and increased access to vaccinations,” a March 2, 2021 letter from the St. Vincent Hospital Board of Trustees read.
Jackson concurred. She said the hospital “never ran out of PPE” and, in fact, had 11,000 rain ponchos that it never had to deploy for use. She also said the hospital had “minimum” staff-to-staff and patient-to-staff infections compared to some peer institutions.
“Everybody had challenges, but I would say that we did better than a lot of the hospitals that I have talked to in the state and across the country,” Jackson said. “Having adequate PPE, having tight at times but appropriate staffing, and minimal staff infections, we did pretty well.”
Nurses nevertheless put in long hours in a physically and mentally demanding situation, often with highly acute patients.
And in the midst of COVID - and a day after nurses unanimously rejected a proposed contract and also after the state announced almost $1 billion to shore up the health care industry in response to COVID, St. Vincent Hospital announced furloughs.
The hospital said the furloughs were voluntary and that more workers applied than were required. Nurses disagreed with this characterization.
But coming amidst contract disputes and in the midst of a health care crisis, nurses said they felt betrayed.
“The pandemic just made us realize that things were only going to get worse for us if we didn’t take a stand now,” Ritacco said. “Employers like ours looked at what we were able to do during the pandemic and decided that that would become our new norm, and we knew we could not perform at those crises level without really harming people in the process, and we were not going to accept that going forward...That experience just solidified for us that they were not to be trusted.”
Outside observers agree about the impact of COVID.
“I think (COVID) is really what pushed the St. Vincent’s issue to a head,” said Despain. “They already had the main dispute of staffing, then the hours put in by nurses went up because of COVID, and they just couldn’t come to an agreement.”
Juravich said the COVID “crisis” has put “all kinds of pressures on the health care industry.”
“There’s been a great need for health care because of COVID, but it’s also got in the way of hospitals doing elective surgeries, which is where they make profits,” Juravich said. “We’ve also seen a lot of activism and militarism from nurses and advocacy.”
“I think that we’ve seen across the country, nurses, and people in health care standing up and saying we deserve to be treated well,” Juravich continued. “I think that’s playing out in Worcester. Nurse-to-patient ratios do matter, and they matter a lot to their ability to do good work.”
Monica Carney, a professor of economics at the College of the Holy Cross who specializes in health care and labor, agreed that staffing ratios matter.
“I think that it’s become more apparent that support and staffing ratios matter in health care, particularly that’s important because of the pandemic,” Carney said in an interview.
Nursing shortage
But nurse-to-patient ratios are hard to fill when there is a shortage of nurses.
“Right now is a wonderful time to be entering the nursing workforce: I believe it’s a buyer’s market for nurses,” Pat Creelman, a professor of nurse education at Quinsigamond Community College, said. “Many facilities are offering sign-on bonuses because the number of nurses is so low, even for new graduates...the jobs are plentiful.”
Ethan Roden, director of human resources and operations for MSG Staffing in Worcester, agreed.
“Nurses have their pick in this present market,” Roden said in an email. “Everyone is sourcing the same candidates for the same positions. Nurses have the ability to choose where they would like to work and at what price. Nurses will not settle for less.”
According to the Bureau of Labor Statistics’ Occupational Outlook Handbook, employment of registered nurses is projected to grow 7% from 2019 to 2029, “faster than the average for all occupations.”
“Growth will occur for a number of reasons, including an increased emphasis on preventive care; increasing rates of chronic conditions, such as diabetes and obesity; and demand for health care services from the baby-boom population, as this group leads longer and more active lives,” according to the BLS.
The extent of the local shortage is difficult to determine, however.
According to a Department of Public Health spokesperson, the executive director of the state’s Board of Registration in Nursing said “she didn’t have any information or data that would be useful to share for your story.” Two queries for an interview with a representative of the Massachusetts Health and Hospital Association for this story yielded no results. Moreover, Creelman said she “can’t really comment on St. Vincent’s and don’t want to.”
However, Creelman said that in 20 years at QCC, the ebb and flow of nurses is at a low.
“Probably, we’re in a better place than we were in 2005-2006. However, I’m finding those conversations starting up again in facilities about needing to find creative ways to attract staff,” Creelman said.
COVID also didn’t help the staffing shortage on the other end.
“I believe COVID has had a negative effect on nursing, in that a lot of people have chosen to retire because of the COVID pandemic, so that has also led to the shortage in nursing,” Creelman said.
Jackson said the workforce experienced both many workers deciding to retire early and workers taking leave because the lockdown gave them additional responsibilities at home.
Juravich also said nurses’ complaints about unsafe staffing and difficult working conditions didn’t help the shortage.
“One of the bigger issues is not how many people are coming into the pipeline but how many are leaving because of these types of working conditions,” Juravich said.
“If companies want to retain nurses, then they have to hold up the conditions and staffing that make it possible to be working,” Juravich continued. “There’s not a reserve army out there in Central Mass. or anywhere in the country of nurses who are willing to go anywhere and work for any company.”
Corporate ownership
Particularly a company where a lack of trust, and as Ritacco said earlier, exists between nurses and leadership. The nurses took a vote of no confidence in Jackson’s leadership in May 2020, and the trust has only further eroded since the beginning of the strike as the hospital’s spending on police details and travel nurses has nurses questioning the hospital’s priorities.
“With all the money wasted, they could have given it to the community, given it back to the hospital and hired the nurses we need,” Nurse Chris Cuthbert said Wednesday, citing an MNA estimate that Tenet has spent more than $75 million on the strike. Jackson has disputed MNA estimates as too high but not cited an exact cost of the strike.
“Tenet could have been a hero,” Cuthbert said. “Instead they’re a zero.”
Then there is the fact that this is the second go-around between the company and striking St. Vincent nurses.
It’s also pretty easy to criticize Tenet - a for-profit health care company with 65 hospitals and approximately 450 outpatient centers and “additional sites of care” that has paid $1.7 billion in penalties since 2000, according to Good Jobs First, a national policy resource center.
Again, the pandemic exacerbated the criticism.
“The apparent greed of Tenet Healthcare during an unprecedented public health emergency and economic crisis is astounding, particularly in light of the billions in taxpayer assistance received by your company, and the ongoing failure to address the concerns of its frontline health care workers,” U.S. Sens. Elizabeth Warren and Ed Markey and U.S. Reps. James P. McGovern and Lori Trahan wrote in a June 29 letter to Tenet’s CEO Ronald A. Rittenmeyer.
The letter noted that Tenet sought more than $2 billion in loans and grants from the federal government, “an effort you admitted was aimed at “maximizing [Tenet’s] cash position.” Moreover, despite the pandemic, Tenet reported annual earnings over $3.1 billion in 2020, and their stock price has increased fivefold from March 20, 2020, to June 16, 2021, according to the letter. The chain also produced a $97 million profit in the first quarter of 2021. Meanwhile, from April to June 2020, Tenet "slashed hospital spending by 11% or $377 million, while receiving more than $850 million of federal stimulus money," the letter said, citing a Tenet earnings release.
“Symbolically right now, and far beyond Worcester and the lines of the commonwealth, there is a sense that these larger corporations are sometimes not in the best interest of nurses and patients,” Juravich said. “I don’t know there is a lot of love for Tenet in Worcester.”
Juravich said that this corporate structure can lead to a disconnect between the goals of a for-profit company and the goals of nurses at the bedside.
“St. Vincent, like much of health care, has seen lots of buyouts and takeovers of smaller community hospitals, and it’s all well and good that you may want to run the hospital this way but we have traditions and practices, and our patients have needs that we need to fill on a local basis,” Juravich said. “Sometimes health care is not part of a larger strategic plan, sometimes it depends on what happens on the floors.”
Despain said this disconnect between corporate and local management is “a big part of the tension here.”
“You have a number of nurses who fundamentally don’t agree with the type of management put over them by Tenet,” Despain said. “Tenet meanwhile is trying to provide a profitable business and provide care. I don’t think Tenet is trying to not provide care; but when you do it on a shoestring, it becomes very precarious.”
Nurses concur, repeatedly referring over the course of the strike to St. Vincent Hospital as a Worcester - not a Tenet - institution.
“This is our community hospital,” nurse Dominique Muldoon said in an interview earlier this month.
Community members and politicians have also rallied to the nurses’ cause. As Schildmeier pointed out, nobody has been holding vigils or displaying lawn signs for Tenet.
But is it perhaps too easy to paint Tenet as the big, bad corporate Goliath?
“I prefer to call it a taxpaying hospital rather than a for-profit hospital,” Jackson continued. “We are quite important to the Worcester economy, not just for jobs we provide, but the tax revenue we provide for the city and the quality care we provide for the community.”
Jackson noted that the hospital was the third-largest taxpayer in the city, paying at least $13 million annually to city coffers.
“We provide excellent care and at a reasonable cost and I think Tenet has been a good steward of its hospital,” Jackson said.
The question is whether Tenet has been a good steward of its nurses.
Albani, back at the strike, didn’t think so.
She said that since Tenet took over at the hospital in 2013 the amount of supplies has decreased, there have been cheaper supplies, positions have been cut, vacant positions have not been filled soon enough, and staffing guidelines haven't been followed.
“This strike could be settled: The nurses that have been out here picketing are the hospital’s best asset as far as loyalty, integrity and commitment to patient safety,” Albani said. “They had the money, and they blew it.”
No comments:
Post a Comment