PATHOLOGY/VIROLOGY
Report calls for regulations around dangerous pathogen research

March 7, 2024 – In recent years, concerns have been raised about the dangers of research on risky pathogens—the kind that could trigger a pandemic. In February, a task force convened by the Bulletin of Atomic Scientists released a report that makes recommendations on strategies for conducting such research, calling for stronger oversight. Harvard T.H. Chan School of Public Health’s Marc Lipsitch served on the task force. Lipsitch, professor of epidemiology and director of the Center for Communicable Disease Dynamics at Harvard T.H. Chan School of Public Health, discusses key takeaways from the new report.
What was the impetus behind this report?
There’s a growing realization in many quarters that while most biological research is completely safe or poses risks only to a small number of individuals involved in research, there’s a very small subset of biological research that poses risks beyond the individuals involved, because it involves the potential for an accident or a deliberate misuse that could lead to widespread transmission of the agent being studied.
The issue is quite polarized between some individuals who suggest that scientists should be able to regulate themselves and there’s no need for outside oversight, and others who have proposed, and in some cases enacted, bans on whole categories of research at the state level, for example in Florida.
The task force was by design a very international, cross-disciplinary group, including virologists, epidemiologists, biosafety experts, social scientists, a philosopher, and others. The idea was to find some kind of common ground on what is the scope of research that needs to be more carefully scrutinized and what that scrutiny might be.
What was amazing about the process was that, despite different backgrounds and in some cases different starting positions, we were able to come to agreement on a set of principles that, if taken seriously by those designing policies, really has some teeth.
What are some key takeaways from the report?
The most important thing is that this group acknowledges that there is a scope for special regulation of the types of research that risk a pandemic. This sort of research is a small subset, but a particularly risky subset. We also state that this is not a matter for science to self-regulate. It’s a matter for public consideration, and the public has a right to be a part of the process.
The second key takeaway is that the report gets specific about the types of research that are of top concern: research with known pandemic pathogens; research that could somehow create a pandemic pathogen; and research with pathogens of unknown risk.
A third takeaway has to do with equity, which has been lacking in the discussion in the past. It is an unfortunate but true fact that the benefits of scientific research come first, in most cases, to the developed world, and only later, if at all, to the rest of the world. That means that research that promises potential biomedical benefits at the risk of possibly starting a pandemic is just further disadvantaging groups that have already been disadvantaged, because they don’t have first crack at the benefits and are likely to face disproportionate risks.
Another key principle articulated in the report is that researchers should look as hard as possible for safer alternatives to risky research.
Was there anything particularly controversial or tricky as you and the other task force members worked on the report?
The particulars about the kinds of risks, how big they are, and what the benefits need to be—that did require some judgment. There was a lot of discussion in the group about how strongly to assert the need for a public health benefit to offset a public health risk. My preferred interpretation is that the scientific benefit alone is not good enough—that you need a clear path to a public health benefit before you should accept any risk to public health.
How do you foresee the report’s recommendations being implemented?
You would have to have some kind of local, national, or institutional implementation. But the principles outlined in the report are global and the enforcement or the incentives should be global. Journals would play an important role. For example, if a researcher did something that didn’t get proper scrutiny, a journal should not accept it for publication.
What’s happening in the U.S. regarding oversight of risky pathogen research?
At the moment, there is a panel within the Department of Health and Human Services that reviews some of this research, but their identities and deliberations are secret. Our task force would like to see greater transparency in the process. In the meantime, the federal government is considering updating the framework that governs this review process. I hope that the update comes out soon and is consistent with the kind of recommendations we’ve outlined in this report.
What are your thoughts on the level of risk the word faces right now from a lab leak that could start another pandemic?
I don’t know the magnitude of the risk. I just know that it’s our responsibility to minimize it.
Photo: iStock/pkujiahe
Researchers reveal how a virus hijacks insect sperm: May help control disease vectors and pests
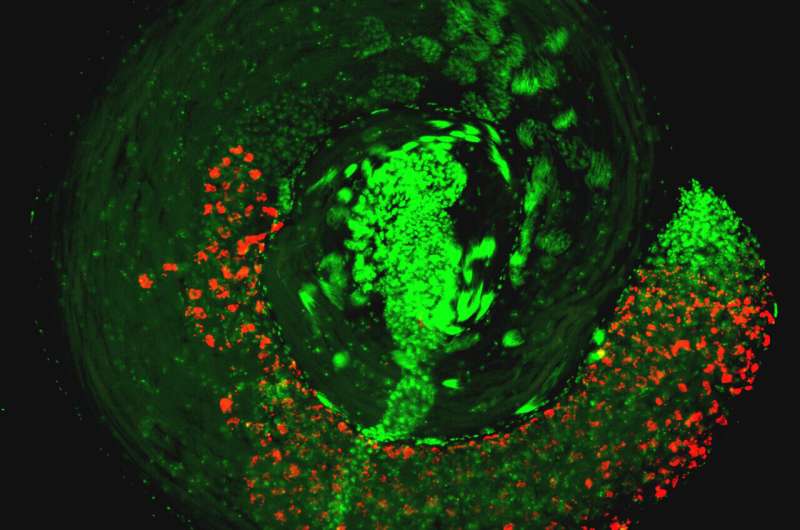
A widespread bacteria called Wolbachia and a virus that it carries can cause sterility in male insects by hijacking their sperm, preventing them from fertilizing eggs of females that do not have the same combination of bacteria and virus.
A new study led by microbiome researchers at Penn State has uncovered how this microbial combination manipulates sperm, which could lead to refined techniques to control populations of agricultural pests and insects that carry diseases like Zika and dengue to humans.
The study is published in the journal Science.
"Wolbachia is the most widespread bacteria in animals and lives symbiotically within the reproductive tissues of about 50% of insect species, including some mosquitos and flies," said Seth Bordenstein, professor of biology and entomology, director of the One Health Microbiome Center at Penn State, and one of the leaders of the research team.
"Wolbachia has genes from a virus called prophage WO integrated into its genome. These genes—cifA and cifB—allow the bacteria to remarkably manipulate sperm and quickly spread through an insect population for their own good."
When a male and female insect that both have Wolbachia mate, they successfully reproduce and pass on the bacteria. But when a male with Wolbachia mates with a female with no Wolbachia, the sperm are rendered lethal to the fertilized eggs, succumbing them to death. This system cunningly increases the proportion of offspring with Wolbachia and the virus in the next generation, because females with the bacteria successfully reproduce more frequently than females without.
This system is being used in several ongoing pilot studies across the world to control insect pests and the harmful viral diseases they carry. For example, to control a population of agricultural or human pests that do not have the bacteria, scientists release males with Wolbachia in order to crash the population.
"One of Wolbachia's superpowers is that it blocks pathogenic RNA viruses such as Zika, dengue and chikungunya virus, so mosquitos with Wolbachia do not pass these viruses on to people when they bite," Bordenstein said.
"So, releases of both male and female mosquitos with Wolbachia in an area where it isn't already present leads to replacement of the population with mosquitos that can no longer pass on a viral disease. The World Mosquito Program is now using Wolbachia to control viruses in 11 countries. With this study, we reveal the underlying mechanics of how this process works so we can fine-tune the technique to expand its scope in vector control measures."
Wolbachia's prophage WO genes code for proteins that interfere with normal development of sperm cells. These proteins impact a critical transformation during sperm development, when the sperm's genome is repackaged and the sperm changes from a canoe-shape into a more refined needle-like shape.
"This shape change is incredibly important to the success of sperm, and any interference can impact the sperm's ability to travel in the female reproductive tract and successfully fertilize the egg," said Rupinder Kaur, assistant research professor of biology and entomology at Penn State and the other leader of the research team.
"The transition is highly conserved in almost everything from insects to humans. Defects in this process can also cause male sterility in humans."
According to the researchers, sperm is particularly prone to DNA damage and repair during this transition. In this study, they found that sperm exposed to Wolbachia, or the Cif proteins alone, had an elevated level of DNA damage at this stage. The DNA damage, if not repaired in a timely fashion, can result in abnormal sperm genome packaging, male infertility and embryonic inviability.
"These results confirmed the impact of Wolbachia and Cif proteins at this stage of sperm development, but we still wanted to know what was happening at earlier stages to trigger these changes," Kaur said.
"We conducted a series of tests to explore the structure and biochemical function of the Cif proteins and found that they can cleave messenger molecules called long non-coding RNA, which sets the stage to interfere with downstream development and function of the sperm."
The researchers used fruit flies with Wolbachia to test the potential link between the bacteria and long non-coding RNA. They found that Wolbachia—or the Cif proteins alone—reduced the amount of these RNAs. Additionally, mutant flies with reduced expression of these RNAs in conjunction with Wolbachia had elevated levels of embryonic inviability because it augmented the defective transition process of sperm development.
So, Kaur explained, the virus proteins control sperm by depleting the long non-coding RNAs required for a normal sperm function.
"Long non-coding RNAs do not make any proteins themselves, but they can have profound impacts on regulating the function of other genes required for sperm development," Bordenstein said.
"By altering this non-coding part of the genome, we found that Cif proteins start impacting sperm right from the earliest stages of development. Wolbachia's prophage WO genes act like master puppeteers, manipulating sperm development in a way that allows their genes and the symbiotic bacteria to quickly spread through arthropod populations."
Because the process of sperm development looks similar across the animal kingdom, the researchers said that knowledge of this process could lend insight into sterility challenges in humans as well as inform new control methods of harmful insect populations.
"Now that we have reverse engineered this process, we can fine-tune methods of population control with Wolbachia that are already in use," Kaur said.
"We plan to take advantage of this knowledge to augment currently existing disease vector and pest control methods, and perhaps emulate the technique without Wolbachia or virus proteins in the long-term."
More information: Rupinder Kaur et al, Prophage proteins alter long noncoding RNA and DNA of developing sperm to induce a paternal-effect lethality, Science (2024). DOI: 10.1126/science.adk9469. www.science.org/doi/10.1126/science.adk9469
Journal information: Science
Provided by Pennsylvania State University Fight against Zika, dengue get boost from reliable spread of bacteria
Deadly Diseases That Plagued People in Ancient Times are Similar to Those of Today
In a time before modern medicine, humanity was plagued with a host of diseases that are now easily cured or prevented. But some are still with us even today.
For many people in the ancient world, life was no casual stroll around the Forum. Today, many diseases can be treated with modern medicine or prevented entirely, thanks to the development of myriad vaccines to help rid us of the risk of infection (though major inequalities still mean such lifesaving shots are not available to all).
In ancient times, however, these advances simply were not available, making disease an ever present and deadly risk. Kyle Harper, professor of classics and letters at the University of Oklahoma, says that in ancient times life expectancies were so low in part because infectious diseases were such a powerful force.
“They didn't have the biomedical and public health resources that we enjoy today,” he adds. Healthcare to some degree did exist in the ancient world and medical advances were made, but treatment often revolved around dubious remedies, charms, and superstitions
“The class of diseases that are caused by some kind of microbial invader were one of the most fundamental facts shaping every premodern society,” Harper says.
Tuberculosis and Malaria in Ancient Times
Today, the average global life expectancy is around 70 years of age and continues to increase, but centuries ago, that was hardly the case. In ancient Egypt, it’s believed that the average age at death was as low as 19, mainly due to high infant death rates. The average lifespan of a man is thought to have been around 25. In ancient Greece and Rome, people fared little better as some estimates place the expectancy range between 20 and 35 years.
Attributing to these low life spans, many of the diseases that ancient peoples faced are still recurrent health problems today. Tuberculosis, for example, has ravaged human populations for thousands of years. Egyptian mummies from around 2400 B.C.E. show deformities similar to TB and ancient texts from China and India may refer to it, according to research.
The disease was known as phthisis to the ancient Greeks and the physician Hippocrates reports that many in his homeland succumbed to the illness. Today, over a million people continue to die of TB each year, even though it is both curable and preventable.
Malaria too was likely endemic in ancient Egypt and Nubia, alongside other diseases such as leishmaniasis and schistosomiasis. Two mummies buried around 3,500 years ago likely died of malaria, making them the two earliest known cases of the mosquito-borne disease.
It’s also known that malaria was prevalent in certain regions of the Roman Empire and DNA evidence shows that the malaria was present across Italy in ancient times.
Read More: What Is Hydrophobia and What Causes It?
A range of other diseases hammered ancient civilizations, including cancer, which Hippocrates described, ultimately giving it its name. Similarly, one of the first descriptions of rabies dates back to Greece around 500 B.C.E.
The Roman writer Pliny the Elder describes how those who are bitten by dogs with “canine madness” develop a deadly horror of water, and outlines curious remedies to combat the disease.
Parasites and Pandemics

On top of this massive health burden came others, such as gastrointestinal diseases and parasites such as worms, the impact of which are easy to underestimate, says Harper. Studies indicate that people living in the ancient world were regularly exposed to and riddled with different kinds of intestinal worms.
Read More: The Biggest Parasite Can Grow Up to 30 Feet Long, and Live in Your Stomach
Pandemics also rocked the ancient world. Back in 430 B.C.E., a plague hammered the besieged city of Athens. Over the course of three years, it’s estimated that as many as 100,000 people may have died, representing around one quarter of the city’s population at that time. What caused this particular plague remains somewhat of a mystery.
“The Roman world seems to have experienced a number of really explosive, consequential pandemic disease events,” adds Harper, who has authored books on that same subject.
The Antonine Plague – which occurred between 165 and 180 C.E. – is estimated to have killed around 2,000 people per day in Rome at its peak, even claiming the life of Lucius Verus, co-emperor alongside Marcus Aurelius. It’s unclear what caused the outbreak, says Harper, but suggestions include measles or an ancestral form of smallpox.
Similarly, the Plague of Cyprian occurred between 250 and 270 C.E. It originated in Ethiopia before spreading across the Mediterranean region and beyond; its death toll may have reached as high as 5,000 people per day in Rome, according to estimates. Like the Antonine Plague before it, there is speculation about its cause.
Harper says that it may have been viral hemorrhagic fever, while other possibilities include typhus, measles or meningitis. “Until we get DNA evidence, we are going to have trouble saying what caused the plague,” he notes.
Another Plague, Same as the Black Death
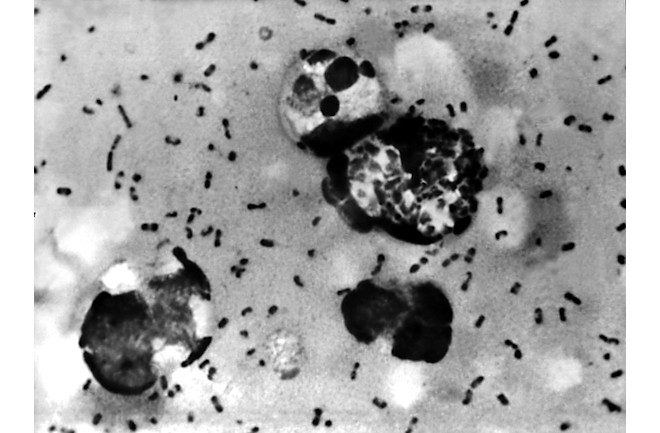
Such evidence does exist for the later, and far more devastating, Plague of Justinian. This erupted in 541 C.E. and continued to claim lives across the Mediterranean for over 200 years.
“The Plague of Justinian in the 540s is the only one where we know with absolute certainty what caused it,” Harper says. “It was bubonic plague.”
Spread by black rats, this plague is the same culprit behind the infamous Black Death that rocked Medieval Europe between 1347 to 1351, killing millions of people. Harper describes it as “the most explosive pandemic disease in human history.”
By the time the outbreak ended, it’s believed that between 25 to 50 million may have died across the Mediterranean, though this is debated.
Read More: Scientists Reveal the Black Death’s Origin Story
Article Sources
Our writers at Discovermagazine.com use peer-reviewed studies and high quality sources for our articles, and our editors review for scientific accuracy and editorial standards. Review the sources used below for this article:
Centers for Disease Control and Prevention. Diseases You Almost Forgot About (Thanks to Vaccines).
National Library of Medicine. The contribution of vaccination to global health: past, present and future.
World Health Organization. Vaccine Equity.
World History Encyclopedia. Medicine in the Ancient World.
World Health Organization. GHE: Life expectancy and healthy life expectancy.
World Economic Forum. Charted: How life expectancy is changing around the world.
University College London. Old age in ancient Egypt.
Kelsey Museum. Life, Death, and Afterlife in Ancient Egypt.
Frontiers. Editorial: Health related quality of life inequalities.
National Library of Medicine. The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus.
ATS Journals. The Masterful Description of Pulmonary Tuberculosis by Soranus of Ephesus (c. 98–138 A.D.).
World Health Organization. Tuberculosis.
Britannica. Malaria through history.
National Library of Medicine. The history of leishmaniasis.
National Library of Medicine. Epidemiology of Schistosomiasis in Egypt: Travel through Time: Review.
National Library of Medicine. Plasmodium falciparum in Ancient Egypt.
Oxford Academic. Malaria and Rome: A History of Malaria in Ancient Italy.
Current Biology. Plasmodium falciparum malaria in 1st–2nd century CE southern Italy.
National Library of Medicine. [Diseases in the ancient world].
American Society for Microbiology. The Ancient Curse: Rabies.
National Library of Medicine. The plague of Athens: epidemiology and paleopathology.
Princeton University Press. The Fate of Rome: Climate, Disease, and the End of an Empire.
World History Encyclopedia. Antonine Plague.
Britannica. Lucius Verus.
World History Encyclopedia. Plague of Cyprian, 250-270 CE.
Centers for Disease Control and Prevention. What are VHFs?
Britannica. Black Death.
No comments:
Post a Comment