Funding will help further development of bacteriophages to combat disease on a commercial scale
Pioneering work to develop effective and safe bacteriophages to combat disease has received an £800,000 boost.
Grant and Award AnnouncementIMAGE:
PROFESSOR MARTHA CLOKIE (LEFT) AND DR ANISHA THANKI
view moreCREDIT: UNIVERSITY OF LEICESTER
Pioneering work to develop effective and safe bacteriophages to combat disease has received an £800,000 boost.
The grant from the Biotechnology and Biological Sciences Research Council (BBSRC), is aimed at advancing the production of phages to combat disease in the veterinary field and bring them to market.
It has been awarded to Professor Martha Clokie, the Director of the Leicester Centre of Phage Research, and Dr Anisha Thanki who earlier this year successfully developed a bacteriophage ‘liquid’ product to prevent Salmonella in broiler chickens.
The latter will now be used as a case study to advance ways in which this novel medicine can successfully and safely be produced in larger scales to meet UK guidelines.
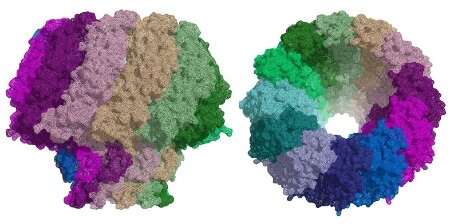
Bacteriophage are viruses that infect bacteria and kill them. They are naturally occurring in the environment around us and can be found where high numbers of bacteria lurk. They have been identified by the UK Government and World Health Organisation as having great potential to prevent and treat infections.
Researcher, Dr Anisha Thanki helped develop the product to prevent Salmonella and will continue with this next stage.
She said: “We know that the development of bacteriophages will help counter growing resistance to existing antimicrobials. If a product such as this was eventually commercialised, it could save the farming industry billions of pounds each year while preventing Salmonella from entering our food chain – something which infects around 91,000 people in the EU every year.
“However, at present we have an effective product but no known way to bring it into wider commercial use. The work we’re doing is so novel that protocols and regulations don’t yet exist to allow that to happen. We’re very excited that this funding will allow us to translate this work to establish how to use phages effectively at a much larger scale and within UK regulation guidelines.
“Once we do this, we aim to have a successful blueprint to enable other effective phage products to be brought to the commercial market.”
Work on the two-year project begins early next year and will take place in collaboration with Dr Robert Atterbury from the University of Nottingham’s School of Veterinary Medicine and Science.
Dr Thanki added: “Working with the school will allow us to develop further models to study phage production on a larger scale and test production protocols to ensure its efficacy and safety.”
Dr Robert Atterbury, Associate Professor in Microbiology at the University of Nottingham said: “Antimicrobial resistance is one of the key global public health challenges of the 21st century. Bacteriophages show great promise in the treatment of infections caused by multidrug resistant bacteria in animals and people. This exciting project, supported by the BBSRC, will allow us to address some of the key hurdles currently preventing their wider use in the agrifood sector and beyond.”
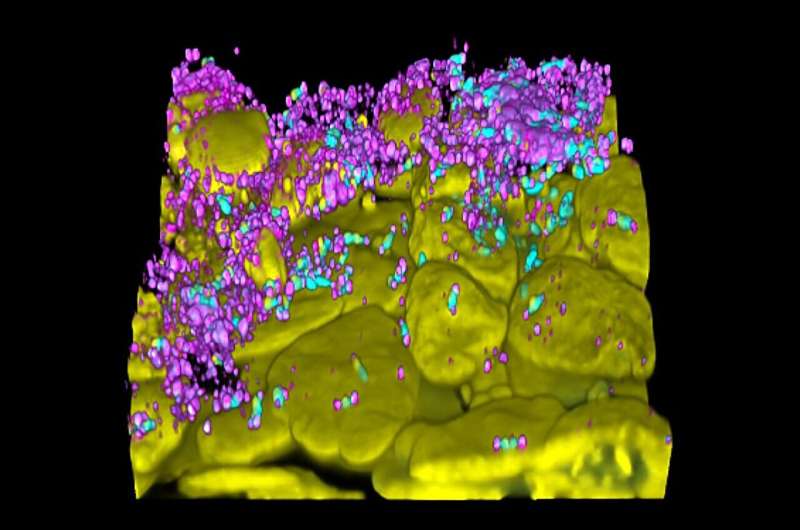
Bacteriophage used within the Salmonella trial, published in scientific journal, Emerging Microbes and Infections, was developed in the University’s pioneering new Leicester Centre for Bacteriophage Research which is studying bacteriophage-based products to prevent and treat bacterial infections in humans, animals and agriculture.
DOI 10.1080/22221751.2023.2217947
SEE