Harnessing bacteriophages as targeted treatments for drug-resistant bacteria
As antibiotic resistance becomes an increasingly serious threat to our health, the scientific and medical communities are searching for new medicines to fight infections. Researchers at Gladstone Institutes have just moved closer to that goal with a novel technique for harnessing the power of bacteriophages.
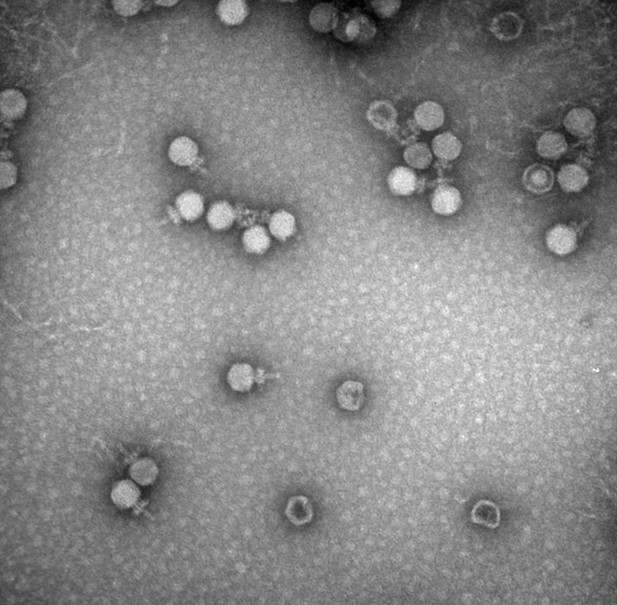
Bacteriophages, or phages for short, are viruses that naturally take over and kill bacteria. Thousands of phages exist, but using them as treatments to fight specific bacteria has so far proven to be challenging. To optimize phage therapy and make it scalable to human disease, scientists need ways to engineer phages into efficient bacteria-killing machines. This would also offer an alternative way to treat bacterial infections that are resistant to standard antibiotics.
Now, Gladstone scientists have developed a technology that lets them edit the genomes of phages in a streamlined and highly effective way, giving them the ability to engineer new phages and study how the viruses can be used to target specific bacteria.
"Ultimately, if we want to use phages to save the lives of people with infections that are resistant to multiple drugs, we need a way to make and test lots of phage variants to find the best ones," says Gladstone Associate Investigator Seth Shipman, PhD, the lead author of a study published in Nature Biotechnology. "This new technique lets us successfully and rapidly introduce different edits to the phage genome so we can create numerous variants."
The new approach relies on molecules called retrons, which originate from bacterial immune systems and act like DNA-production factories inside bacterial cells. Shipman's team has found ways to program retrons so they make copies of a desired DNA sequence. When phages infect a bacterial colony containing retrons, using the technique described in the team's new study, the phages integrate the retron-produced DNA sequences into their own genomes.
The enemy of your enemy
Unlike antibiotics, which broadly kill many types of bacteria at once, phages are highly specific for individual strains of bacteria. As rates of antibiotic-resistant bacterial infections rise-;with an estimated 2.8 million such infections in the United States each year-;researchers are increasingly looking at the potential of phage therapy as an alternative to combat these infections.
"They say that the enemy of your enemy is your friend," says Shipman, who is also an associate professor in the Department of Bioengineering and Therapeutic Sciences at UCSF, as well as a Chan Zuckerberg Biohub Investigator. "Our enemies are these pathogenic bacteria, and their enemies are phages."
Already, phages have been successfully used in the clinic to treat a small number of patients with life-threatening antibiotic-resistant infections, but developing the therapies has been complex, time-consuming, and difficult to replicate at scale. Doctors must screen collections of naturally-occurring phages to test whether any could work against the specific bacteria isolated from an individual patient.
Shipman's group wanted to find a way to modify phage genomes to create larger collections of phages that can be screened for therapeutic use, as well as to collect data on what makes some phages more effective or what makes them more or less specific to bacterial targets.
"As the natural predators of bacteria, phages play an important role in shaping microbial communities," says Chloe Fishman, a former research associate at Gladstone and co-first author of the new study, now pursuing her graduate degree at Rockefeller University. "It's important to have tools to modify their genomes in order to better study them. It's also important if we want to engineer them so that we can shape microbial communities to our benefit-;to kill antibiotic-resistant bacteria, for example."
Continuous phage editing
To precisely engineer phage genomes, the scientists turned to retrons. In recent years, Shipman and his group pioneered the development and use of retrons to edit the DNA of human cells, yeast, and other organisms.
Shipman and his colleagues began by creating retrons that produce DNA sequences specifically designed to edit invading phages-;a system the team dubbed "recombitrons." Then, they put those retrons into colonies of bacteria. Finally, they let phages infect the bacterial colonies. As the phages infected bacteria after bacteria, they continuously acquired and integrated the new DNA from the recombitrons, editing their own genome as they went along.
The research team showed that the longer they let phages infect a recombitron-containing bacterial colony, the greater the number of phage genomes were edited. Moreover, the researchers could program different bacteria within the colony with different recombitrons, and the phages would acquire multiple edits as they infected the colony.
A platform to screen phages
If scientists already knew exactly what edits they wanted to make to a given phage to optimize its therapeutic potential, the new platform would let them easily and effectively carry out those edits. However, before researchers can predict the consequence of a genetic change, they first need to better understand what makes phages work and how variations to their genomes impact their effectiveness. The recombitron system helps makes progress here, too.
If multiple recombitrons are put into a bacterial colony, and phages are allowed to infect the colony for only a short time, different phages will acquire different combinations of edits. Such diverse collections of phages could then be compared.
"Scientists now have a way to edit multiple genes at once if they want to study how these genes interact or introduce modifications that could make the phage a more potent bacterial killer," says Kate Crawford, a graduate student in the Shipman lab and co-first author of the new study.
Shipman's team is working on increasing the number of different recombitrons that can be put into a single bacterial colony-;and then passed along to phages. They expect that eventually, millions of combinations of edits could be introduced to phages to make huge screening libraries.
"We want to scale this high enough, with enough phage variants, that we can start to predict which phage variants will work against what bacterial infections," says Shipman.
Fishman, C. B., et al. (2024). Continuous multiplexed phage genome editing using recombitrons. Nature Biotechnology. doi.org/10.1038/s41587-024-02370-5.
 Yibao Chen
Yibao Chen Himanshu Batra
Himanshu Batra Junhua Dong
Junhua Dong Cen Chen
Cen Chen Venigalla B. Rao
Venigalla B. Rao Pan Tao
Pan Tao



