More Chinese getting HIV when cases in rest of world are falling. It’s because of ignorance about sex, say experts
DECEMBER 05, 2020 By QIN CHEN SOUTH CHINA MORNING POST
The rising incidence of HIV in China over the past decade runs counter to the global trend of a decline in new cases of the virus.
Huang Haojie
The spread of dating apps and increased mobile phone usage have made it much easier for Chinese people to find potential sexual partners. However, given the lack of proper sex education in schools, this has left young people more vulnerable to contracting HIV — the virus that can cause Aids.
“Those hook-up apps accelerate the spread of the disease,” said Xiao Dong, director of Man Wellness Centre, an HIV testing centre based in Beijing.More from AsiaOneRead the condensed version of this story, and other top stories with NewsLite.
It is not just young people in China at risk of getting HIV through sexual transmission, though. Among older people, endemic loneliness and a lack of sexual literacy have also led to a rapid rise in new infections .
According to China’s Centre for Disease Control and Prevention (CDC), the number of new HIV infections among people over 50 years old rose more than 11-fold between 2007 and 2017, from 2,565 cases a year to 29,860.
Shao Yiming, the CDC’s chief HIV expert, told online news portal Ifeng News this week that one of the oldest patients to contract HIV was 93 years old.
“The person was fine at 91 years old but contracted the disease at 93,” he said.
The rising incidence of HIV in China over the past decade runs counter to the global trend of a decline in new cases of the virus.
The Chinese National Health Commission reported that 131,000 people contracted the disease in 2019. In 2007, the number of new cases was just under 33,000.
In 2020, 95 per cent of the newly infected HIV patients contracted the disease through sex — 70 per cent were heterosexual partners.
By comparison, the United States reported just under 38,000 new cases in 2018.
In 2019, the number of people around the world newly infected with HIV was 1.7 million.
The prevalence of sexually transmitted HIV in China is because of several factors, among them the public’s general lack of sexual knowledge and the proliferation of dating apps .
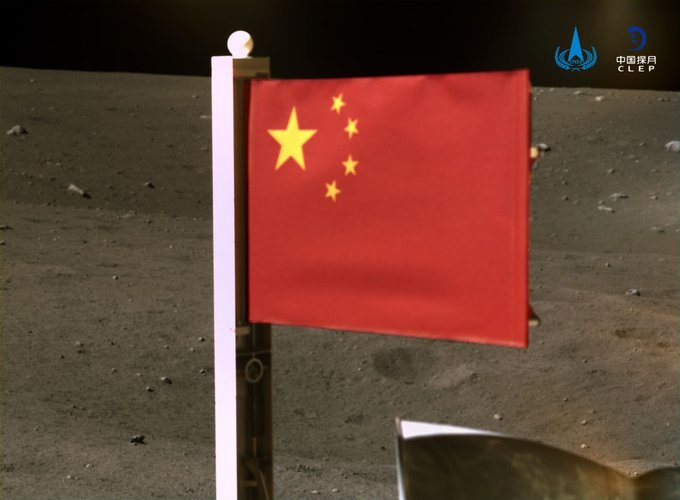
A social worker doing a rapid HIV test for a person in Beijing. Most of the new cases in China are spread through sex. PHOTO: Xiao Dong
Hooking up without sex education
Xiao said he has been urging the Chinese government to get technology companies to do more to protect teenagers and spread knowledge about practising safe sex.
The apps “need to take up these social responsibilities. They have to do it,” said Xiao.
Before new technology changed China’s sex scene, the government consistently shirked its responsibility to provide comprehensive sex education to schoolchildren. Only recently has the government made sex education mandatory for schoolchildren .
For decades, schools in China would either ask students to self-study the reproductive chapter in biology class or give a few sessions about menstrual cycles. Proper sexual behaviour, how to build relationships with the opposite sex, and gender and identity issues were often skipped or there was no teaching about them at all.

Social workers and volunteers promote a 2020 World Aids Day event in the central Chinese city of Wuhan. PHOTO: Huang Haojie
Zhang Renjie, director of Red Ribbon Social Service Centre, a non-governmental group focused on public health and based in the eastern city of Suzhou, said Chinese teenagers “usually don’t know how to refuse sex, or ask for the kind of sex acts they want”.
Huang Haojie, executive director of the Wuhan LGBT Centre in Wuhan, said: “We have heard of patients who contracted HIV as young as 13 and 15. Most teenagers got the disease through sex.”
The number of new HIV patients between the age of 10 and 15 rose from 881 to 3,388 per year between 2007 and 2017, according to the Chinese CDC.
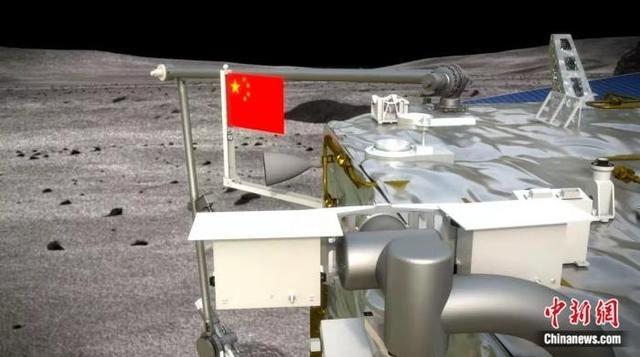
Huang said that when he taught first-year university students about the risks of getting HIV in 2017 and 2018, a school official asked him to avoid talking about specific sex acts or displaying condoms because it was deemed too “sensitive” for the students, who were aged between 18 and 20
.
Huang Haojie from the Wuhan LGBT Centre teaches students about HIV prevention in 2019. PHOTO: Huang Haojie
However, the spread of HIV has forced rapid cultural change. In 2019, that same university begged Huang to discuss sex and condom usage in detail because officials learned the school had a couple of confirmed HIV cases.
In November, China made sex education mandatory for schools as the country grapples with growing problems of sexual harassment, gender inequality and the spread of sexually transmitted infections.
Huang said much of Chinese society believes it is mostly gay people who catch HIV, a debunked misconception. Xiao agreed, and said: “Some schools would tell their students don’t be gay or don’t try out being gay just for fun because of the risk of contracting HIV.”
Lonely, old and looking for love
The other demographic hit hard by China’s growing HIV crisis is the elderly population.
China has urbanised rapidly over the past three decades, and millions of young people have left rural areas and small towns for better job opportunities in the cities. As a result, many old people were left alone at home, and they often experience profound loneliness , which they fill by finding new sexual partners.
Many older people skipped safety precautions because they thought they were not at risk, having assumed HIV is a young person’s disease. Zhang said: “Most older people don’t like to talk about their sex life with others, so they end up using dated knowledge in a time where HIV is spreading much more widely and the risk of contracting is much higher.”

Rapid HIV testing kits can return results within 15 minutes.
PHOTO: Xiao Dong
A silver lining
For some experts, though, the fact that most new HIV cases in China are now sexually transmitted is a reason for celebration.
In the past, China had a problem with poor health standards, which resulted in people contracting HIV when they gave blood or received a blood transfusion .
Huang said the fact most new infections were now sexually transmitted “means now