Study unveils first global dataset for SARS-CoV-2 infections in animals
Structured data on the virus in animals is essential to further our understanding of the COVID-19 pandemic and mitigate its spread at the human-animal interface, according to the authors of the paper published in Scientific Data
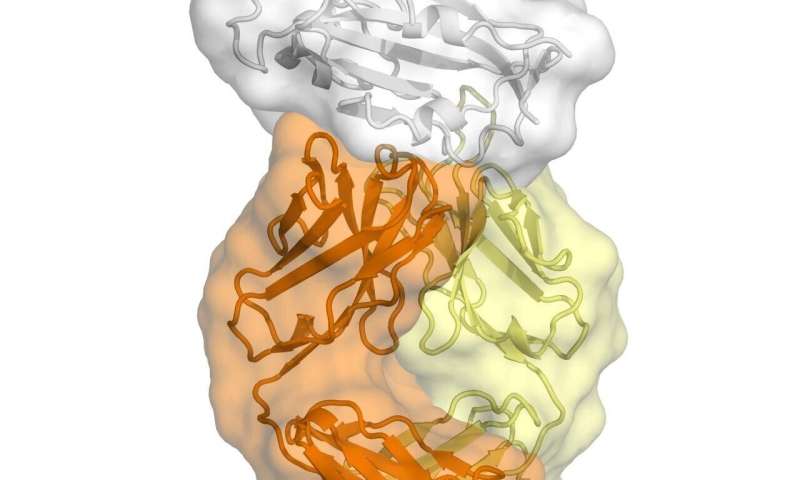
IMAGE: THE DIAGRAM SHOWS THE SARS-COV-2 VARIANTS IDENTIFIED IN THE DIFFERENT ANIMAL HOSTS. THE FIGURE DESCRIBES THE NUMBER OF EVENTS (ONE EVENT MAY INCLUDE ONE OR MORE CASES). view more
CREDIT: NERPEL, A., YANG, L., SORGER, J. ET AL.
[Vienna, July 2022] In a pioneering initiative, a multidisciplinary Austrian team created the most comprehensive global dataset of SARS-CoV-2 infections in animals. Their findings were published Saturday, July 23, in the journal Scientific Data and the epidemiological information is available on a dashboard at https://vis.csh.ac.at/sars-ani/
“There was an urgent need for a global dataset on SARS-CoV-2 events in animals that can be easily imported, processed, and analyzed,” says Amélie Desvars-Larrive, the principal investigator of the study and a researcher at the Complexity Science Hub Vienna (CSH).
The initiative intends to facilitate One Health approaches on SARS-CoV-2. The idea is to create a collaborative approach that recognizes the interdependence of human, animal, and environmental health to obtain optimal health for all.
“To tackle major threats to human health, we need integrated approaches,” points out Desvars-Larrive. “Although animals do not appear to play a significant role in the spread of COVID-19 among people currently, One Health tools that enable the integrative analysis and visualization of SARS-CoV-2 events are critical.”
Two major animal health databases
For the past months, Desvars-Larrive and her team meticulously extracted, combined, and structured information on SARS-CoV-2 cases in animals. They included publicly available data from two major animal health databases: the Program for Monitoring Emerging Diseases (ProMED), a reporting system of the International Society for Infectious Diseases; and the World Animal Health Information System (WAHIS) of the World Organisation for Animal Health.
The unified dataset, called SARS-ANI, feeds a dashboard, which includes an overview of SARS-CoV-2 events in animals worldwide, stratified by species; clinical signs that were allegedly associated with the disease; control measures and outcomes; and a geographical overview of all events. The dashboard is linked to the live dataset available on GitHub.
Answers to current questions
The dataset can help answering some of the many questions regarding SARS-CoV-2 in animals, according to the authors. It shows, for instance, that the number of reported SARS-CoV-2 cases in animals is steadily increasing worldwide. A total of 704 events (one event can include one or more cases that are epidemiologically related) have been reported in 39 countries, across 27 animal species (as of July 25, 2022).
In addition, the team described a high diversity of SARS-CoV-2 variants in the animal hosts, especially in American mink and white-tailed deer. These variants show similarities with human variants. In terms of animal case fatality rates, they are relatively low.
An essential tool
Also, the dataset can be useful for estimating the impact of SARS-CoV-2 on pets, farm animals, wildlife, and conservation programs. In addition, scientists and policymakers can use it to develop guidelines for prevention, risk-based surveillance, and response to SARS-CoV-2.
“We believe the SARS-ANI dataset, with timely and reliable information, can assist in the development of national and international regulations and agreements aiming to reduce the risk of transmission at the human-animal interfaces,” declares Desvars-Larrive, who is also a professor in infection epidemiology at the University of Veterinary Medicine Vienna.
The dataset – a joint effort by experts from CSH, University of Veterinary Medicine Vienna, and Wildlife Conservation Society – will be updated weekly for at least one year. “We also hope to receive new data from researchers around the world to develop it further and expand its use”, says Desvars-Larrive.
CAPTION
The SARS-ANI dashboard gives an easy-to-understand overview of specific aspects of SARS-CoV-2 events in animals and is publicly accessible at https://vis.csh.ac.at/sars-ani/
CREDIT
Nerpel, A., Yang, L., Sorger, J. et al.
The study SARS-ANI: a global open access dataset of reported SARS-CoV-2 events in animals by Afra Nerpel, Liuhuaying Yang, Johannes Sorger, Annemarie Käsbohrer, Chris Walzer, and Amélie Desvars-Larrive appeared in Scientific Data 9 (438) (2022).
The SARS-ANI dashboard gives an easy-to-understand overview of specific aspects of SARS-CoV-2 events in animals and is publicly accessible at https://vis.csh.ac.at/sars-ani/
About CSH
The mission of Complexity Science Hub Vienna is to host, educate, and inspire complex systems scientists dedicated to making sense of Big Data to boost science and society. Scientists at the Hub develop methods for the scientific, quantitative, and predictive understanding of complex systems.
The CSH is a joint initiative of AIT Austrian Institute of Technology, Central European University CEU, Danube University Krems, Graz University of Technology, IIASA, Medical University of Vienna, TU Wien, VetMedUni Vienna, Vienna University of Economics and Business, and Austrian Economic Chambers (WKO).
JOURNAL
Scientific Data
METHOD OF RESEARCH
Data/statistical analysis
SUBJECT OF RESEARCH
Animals
ARTICLE TITLE
SARS-ANI: a global open access dataset of reported SARS-CoV-2 events in animals
ARTICLE PUBLICATION DATE
23-Jul-2022