WOMENS HEALTH
The Menopause Society launches Making Menopause Work™ Initiative
Unique educational and designation initiative based on new science-based Consensus Recommendations to help employers retain workers and recoup $1.8 billion in lost workdays by supporting menopausal women in the workplace
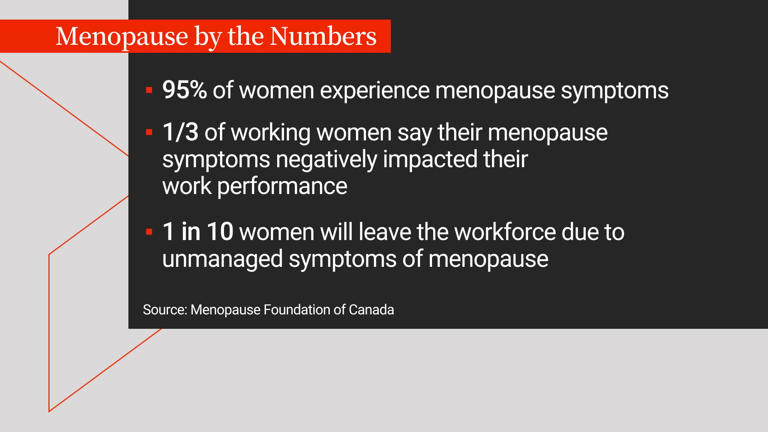
CHICAGO (Sept 13, 2024)—Menopause is a natural life transition occurring when many women are at the “top of their game.” Unsupported menopause symptoms drive up employer healthcare costs and cause roughly $1.8 billion in missed workdays. To help employers retain these valued workers and build cultures of well-being, The Menopause Society launched Making Menopause Work™ based on new science-based Consensus Recommendations. The Recommendations are published online in Menopause, the journal of The Menopause Society.
“More employers—from large corporations to small organizations—are supporting workers during menopause,” Dr. Stephanie Faubion, medical director of The Menopause Society and director of the Mayo Clinic Center for Women’s Health, said today at The Menopause Society’s Annual Meeting in Chicago.
“But more menopause-supportive workplaces are urgently needed,” Faubion continued. “Women ages 50 and older are the fastest-growing demographic group, making essential contributions to society, families, communities, and the paid and unpaid workforces. This is a moment of tremendous opportunity.”
The Menopause Society builds on its 35-year, science-based track record with the creation of Making Menopause Work. The program—which includes a free Employer Guide, an assessment, planning tools, and other resources, with an employer designation program to come—incorporates recommendations based on new scientific consensus recommendations from a multidisciplinary panel of leading medical, legal, and human resource experts.
“Employers need to take menopause symptoms seriously and also know that they’re manageable and temporary,” said Jill K. Bigler, labor attorney at Epstein Becker Green and a member of the advisory panel for the Consensus Recommendations. “Making Menopause Work is a smart, strategic move for employers. It safeguards workers’ opportunities for leadership and financial security. It retains workers and productivity. And it builds a multigenerational workplace where midlife employees hold institutional knowledge, bring calm under stress, and make wise decisions.”
Understanding menopause and creating menopause-responsive workplaces
Menopause, the end of menstrual periods, usually occurs between ages 45 and 55; although perimenopause can start as early as age 35. Symptoms are different for each person. For some, periods become irregular and then stop. Others may experience hot flashes, difficulty sleeping, memory problems, mood disturbances, vaginal dryness, or weight gain.
The Society’s Consensus Recommendations cite a survey by the Society for Women’s Health Research showing that two out of five people had considered looking for or had found a new job because of menopause symptoms. Not only do employers risk losing talent and revenues when they ignore menopause, they also face greater costs for healthcare as well as the cost of replacing and training workers.
Creating a supportive workplace culture is the first step in turning these numbers around. The Employer Guide supports employers, managers, and supervisors to do this, including opening conversations for those who want it, understanding how to hear and support people’s needs, and recognizing menopause as a normal part of life for half the population.
From there, the Employer Guide helps employers update policies, benefits, and environments, including offering the following:
- Health insurance plans that include adequate and affordable coverage for menopause-related care
- Access to adequate bathrooms and flexible breaks to use them—vital for people with heavy or unpredictable bleeding
- Improved ventilation and updated uniforms with breathable, flexible fabrics—a game changer for people experiencing hot flashes
- Quiet work environments and flexible deadlines, which improve focus for people experiencing insomnia, anxiety, or brain fog
- Peer support networks, employee resource groups and employee assistance programs, which can help people know they’re not going through menopause alone
Employers or employees interested in learning more about this important initiative should visit menopause.org/workplace.
The Menopause Society (formerly The North American Menopause Society) is the leading nonprofit organization dedicated to empowering health care professionals to improve the health of women during the menopause transition and beyond. Employers who support Making Menopause Work become part of a movement that includes more than 2,000 health care professionals who have earned The Menopause Society’s Certified Practitioner (MSCP) credential, along with tens of thousands of people who rely on The Menopause Guidebook, the most complete consumer menopause resource available.
Not in the mood for sex after menopause?
A new study suggests that cognitive behavioral therapy could be key in improving sexual function in postmenopausal women
The Menopause Society
CLEVELAND, Ohio (Sept 10, 2024)—Many women report a decline in sexual function, including desire, when transitioning through menopause. Such problems can contribute to poor self-image and negatively affect physical and emotional well-being. A new study suggests that cognitive behavioral therapy may be a safe and effective treatment for mitigating sexual concerns during this period. Results of the study will be presented at the 2024 Annual Meeting of The Menopause Society in Chicago September 10-14.
Partially due to declining estrogen levels, 68% to 87% of peri- and postmenopausal women express sexual concerns. Despite such high prevalence and negative impacts, treatment options–particularly nonpharmacological ones–are quite limited. In response, researchers initiated a small study to evaluate the efficacy of a four-session individual cognitive behavioral therapy protocol for improving sexual functioning (eg, desire, arousal, pain, satisfaction). Secondary objectives included assessing body image, relationship satisfaction, menopause symptoms (such as hot flashes), depression, and anxiety during peri- and postmenopause.
The researchers found that participants in this study experienced a significant improvement in multiple areas of sexual functioning, body image and couple satisfaction, as well as a significant decrease in menopause symptoms, depression, and anxiety, and self-reported overall health. In addition, 100% of participants indicated they were very satisfied with the treatment and that it helped them cope with their symptoms more effectively.
“To our knowledge, this is the first study that has examined the efficacy of a cognitive behavioral therapy protocol specifically aimed to improve sexual concerns experienced during peri- and postmenopause,” says Dr. Sheryl Green, lead study author from McMaster University in Ontario, Canada. “Results suggest that this type of therapy leads to significant improvements across several important sexual concern domains, and we hope this study will provide the basis for larger randomized clinical trials in the future.”
More detailed results will be discussed at the 2024 Annual Meeting of The Menopause Society as part of the Top Scoring Abstract Session presentation titled “Cognitive behavioral therapy for sexual concerns during peri- and postmenopause, a clinical trial.”
“This study is important to women experiencing sexual health related issues and provides their healthcare professionals with another nonpharmacologic treatment option to discuss with their patients,” says Dr. Stephanie Faubion, medical director for The Menopause Society.
Both Drs. Green and Faubion are available for interviews prior to the Annual Meeting.
For more information about menopause and healthy aging, visit the newly redesigned www.menopause.org.
The Menopause Society (formerly The North American Menopause Society) is dedicated to empowering healthcare professionals and providing them with the tools and resources to improve the health of women during the menopause transition and beyond. As the leading authority on menopause since 1989, the nonprofit, multidisciplinary organization serves as the independent, evidence-based resource for healthcare professionals, researchers, the media, and the public and leads the conversation about improving women’s health and healthcare experiences. To learn more, visit menopause.org.