WHO urges the public to avoid routine dental work amid the coronavirus pandemic
Download PDF Copy
By Angela Betsaida B. Laguipo, BSN
Aug 14 2020
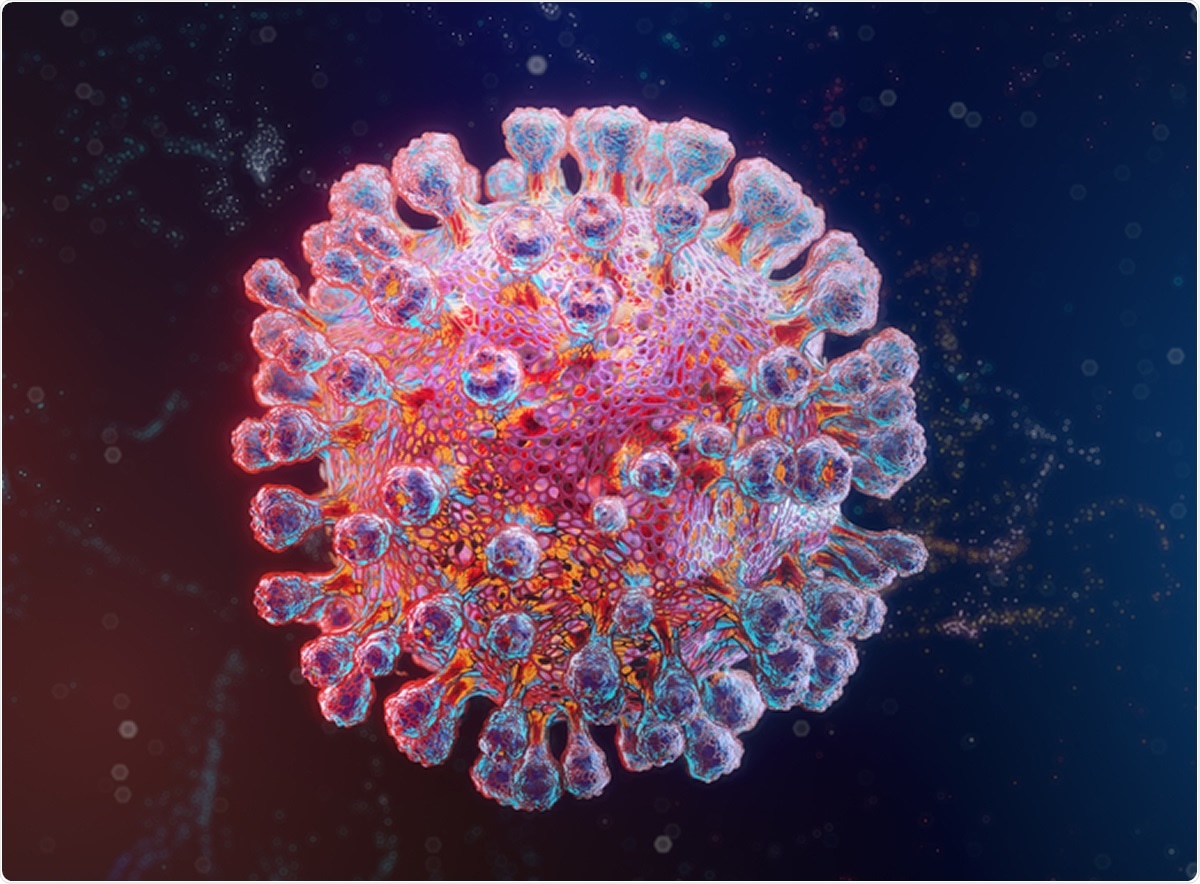
With the cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) skyrocketing globally, the World Health Organization (WHO) is now warning the public to avoid routine dental procedures to reduce the risk of infection.
In a new interim guidance released by the World Health Organization (WHO), the health agency advises that routine non-essential oral health care, which includes dental check-ups, oral prophylaxis, and preventive care, should be delayed until there has been sufficient reduction in SARS-CoV-2 transmission rates from community transmission to cluster cases.
Considerations for the provision of essential oral health services in the context of COVID-19. Image Credit: Willyam Bradberry / Shutterstock
The WHO recommends that patients who do not need urgent dental care to avoid going to the dentist for the meantime, since the global number of SARS-CoV-2 cases has increased to more than 20.77 million, with at least 754,000 lives lost.
“During the COVID-19 pandemic, effective prevention of oral problems and self-care remains a high priority. Patients should be advised through remote consultation or social media channels on maintaining good oral hygiene,” the WHO said.
Further, WHO said that the guidance also applies to other dental procedures, including those for aesthetic purposes. Online consultations are also encouraged to prevent the risk of community transmission, especially that the pandemic is far from over. However, urgent or emergency oral health care interventions can preserve a person’s oral functioning, to secure one’s quality of life, and to manage severe pain.
Virus spread in oral healthcare settings
Today, health experts have identified high-risk areas where the virus can spread from one person to another. Some locations, where there is a heightened risk of spread, including oral healthcare settings like dental clinics, hospitals, public transportation, and buildings with poor ventilation.
The way SARS-CoV-2 spreads happens through direct, indirect, or close contact with those diagnosed with COVID-19. A person who is infected can spread the virus through respiratory droplets or secretions such as saliva.
In dental clinics, the novel coronavirus can be transmitted by three ways – direct transmission through inhalation of droplets produced by talking, coughing, or sneezing, direct transmission through the exposure of mucous membranes like those found in the eyes, nasal area, or oral mucosa, and through the indirect transmission via contaminated surfaces.
Further, oral health care teams work close to the patients’ faces for prolonged periods. Further, the procedures usually performed involve exposure to many body fluids that may harbor SARS-CoV-2, such as saliva and blood.
Dental practice also involves aerosol-generating procedures (AGPs), which are defined as any medical, dental, and patient care procedure that causes the production of airborne particles, which may contain virus particles.
How to contain SARS-CoV-2 in dental care settings?
To contain the spread of SARS-CoV-2 in dental settings, the WHO urges that dentists only perform emergency or urgent oral procedures. Routine dental care, such as dental cleanings, consultations, and preventive care, should be postponed until the pandemic is over or until there is low COVID-19 transmission.
“Urgent or emergency oral health care may include interventions that address acute oral infections; swelling; systemic infection; significant or prolonged bleeding; severe pain not controllable with analgesia; oral health care interventions that are medically required as a pre-intervention to other urgent procedures; and dental/orofacial trauma,” the WHO said.
The WHO also reiterated that dentists should refer patients if they are in doubt to specialized treatment facilities, since addressing the emergency or urgent care appropriately will prevent the need for them to seek treatment at emergency departments of hospitals, reducing the risk of exposure and freeing up space for those who are seeking COVID-19-related care.
The WHO also provided a rundown of how dentists can go about with the pandemic, without risking their health and the health of others. Dentists should screen patients before the appointment through virtual technology or telephone. Also, they should perform triaging when the patient has arrived in the clinic. Make sure that patients seeking urgent care are catered first, and they do not exhibit the symptoms of COVID-19.
Dentists should also develop a remote assessment of their patients to distinguish those seeking urgent or emergency care. The WHO also underlined the importance of disinfection of the clinic, proper infection control practices, improving the clinic’s ventilation, and the wearing of personal protective equipment (PPE) for healthcare workers.
Source:
World Health Organization (WHO). (2020). Considerations for the provision of essential oral health services in the context of COVID-19. https://www.who.int/publications/i/item/who-2019-nCoV-oral-health-2020.1

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
With the cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) skyrocketing globally, the World Health Organization (WHO) is now warning the public to avoid routine dental procedures to reduce the risk of infection.
In a new interim guidance released by the World Health Organization (WHO), the health agency advises that routine non-essential oral health care, which includes dental check-ups, oral prophylaxis, and preventive care, should be delayed until there has been sufficient reduction in SARS-CoV-2 transmission rates from community transmission to cluster cases.
Considerations for the provision of essential oral health services in the context of COVID-19. Image Credit: Willyam Bradberry / Shutterstock
The WHO recommends that patients who do not need urgent dental care to avoid going to the dentist for the meantime, since the global number of SARS-CoV-2 cases has increased to more than 20.77 million, with at least 754,000 lives lost.
“During the COVID-19 pandemic, effective prevention of oral problems and self-care remains a high priority. Patients should be advised through remote consultation or social media channels on maintaining good oral hygiene,” the WHO said.
Further, WHO said that the guidance also applies to other dental procedures, including those for aesthetic purposes. Online consultations are also encouraged to prevent the risk of community transmission, especially that the pandemic is far from over. However, urgent or emergency oral health care interventions can preserve a person’s oral functioning, to secure one’s quality of life, and to manage severe pain.
Virus spread in oral healthcare settings
Today, health experts have identified high-risk areas where the virus can spread from one person to another. Some locations, where there is a heightened risk of spread, including oral healthcare settings like dental clinics, hospitals, public transportation, and buildings with poor ventilation.
The way SARS-CoV-2 spreads happens through direct, indirect, or close contact with those diagnosed with COVID-19. A person who is infected can spread the virus through respiratory droplets or secretions such as saliva.
In dental clinics, the novel coronavirus can be transmitted by three ways – direct transmission through inhalation of droplets produced by talking, coughing, or sneezing, direct transmission through the exposure of mucous membranes like those found in the eyes, nasal area, or oral mucosa, and through the indirect transmission via contaminated surfaces.
Further, oral health care teams work close to the patients’ faces for prolonged periods. Further, the procedures usually performed involve exposure to many body fluids that may harbor SARS-CoV-2, such as saliva and blood.
Dental practice also involves aerosol-generating procedures (AGPs), which are defined as any medical, dental, and patient care procedure that causes the production of airborne particles, which may contain virus particles.
How to contain SARS-CoV-2 in dental care settings?
To contain the spread of SARS-CoV-2 in dental settings, the WHO urges that dentists only perform emergency or urgent oral procedures. Routine dental care, such as dental cleanings, consultations, and preventive care, should be postponed until the pandemic is over or until there is low COVID-19 transmission.
“Urgent or emergency oral health care may include interventions that address acute oral infections; swelling; systemic infection; significant or prolonged bleeding; severe pain not controllable with analgesia; oral health care interventions that are medically required as a pre-intervention to other urgent procedures; and dental/orofacial trauma,” the WHO said.
The WHO also reiterated that dentists should refer patients if they are in doubt to specialized treatment facilities, since addressing the emergency or urgent care appropriately will prevent the need for them to seek treatment at emergency departments of hospitals, reducing the risk of exposure and freeing up space for those who are seeking COVID-19-related care.
The WHO also provided a rundown of how dentists can go about with the pandemic, without risking their health and the health of others. Dentists should screen patients before the appointment through virtual technology or telephone. Also, they should perform triaging when the patient has arrived in the clinic. Make sure that patients seeking urgent care are catered first, and they do not exhibit the symptoms of COVID-19.
Dentists should also develop a remote assessment of their patients to distinguish those seeking urgent or emergency care. The WHO also underlined the importance of disinfection of the clinic, proper infection control practices, improving the clinic’s ventilation, and the wearing of personal protective equipment (PPE) for healthcare workers.
Source:
World Health Organization (WHO). (2020). Considerations for the provision of essential oral health services in the context of COVID-19. https://www.who.int/publications/i/item/who-2019-nCoV-oral-health-2020.1

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.





_Bio.jpg)
_Bio.jpg)
_Bio.jpg)







/https://www.thestar.com/content/dam/thestar/business/2020/08/13/alberta-eyes-cleaner-future-as-hydrogen-superpower/alberta_oil_sands.jpg)