How a decade of privatisation and cuts exposed England to coronavirus

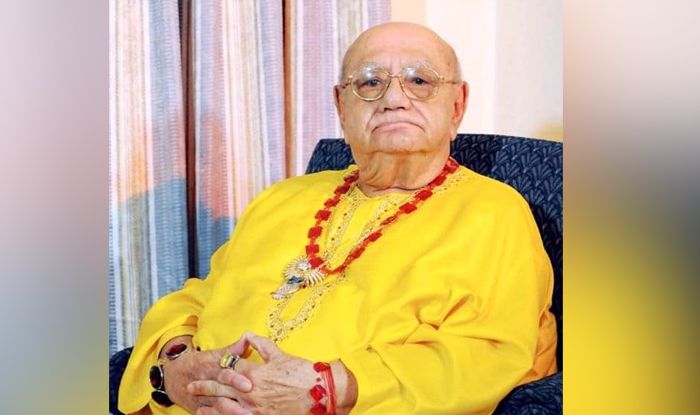
Jason Strelitz at the Covid-19 hub for local authority action in Newham. Photograph: Graeme Robertson/The Guardian
In normal times, a Public Health England (PHE) representative would be expected to contact Strelitz’s environmental health teams if a case of a notifiable disease was found in the area that needed following up, enabling them to set to work tracing contacts and containing an outbreak. But the government had just abandoned community testing and tracing so local authorities were not being contacted at that point.
Newham is among the most deprived boroughs in the country. Like all the public health directors interviewed by the Guardian, Strelitz has deep knowledge of the characteristics of his patch that make its health inequalities so stark and its residents so vulnerable to the disease. About 30,000 people have been identified by the council as being at high risk – many of them over 70, living alone and isolated.
Even now, with large-scale community testing resumed, Strelitz said he was not receiving useful test data from the centralised, privately contracted operation created by Hancock. He also has concerns about the contact-tracing operation being set up.
In addition to the contact-tracing app, the government has once more turned to outsourcing companies, including Serco and Sitel, to recruit and train 25,000 contact tracers. Working on a salary just above minimum wage, the majority will have no medical training. Using scripts, they will contact those who have tested positive, trace people they have been in contact with, and advise them on how to isolate.
“Contact tracing is a sensitive issue – I’m not sure how well it can be done with a remote call centre with no understanding of people’s local context,” Strelitz said.
Dominic Harrison, the director of public health for Blackburn and Darwen, has similar concerns. Speaking earlier this month he said there was “a huge disconnect” between different branches of government, with some functions of the local public health system having been disabled in recent years.
“People like environmental health officers, community and neighbourhood teams, youth services workers – the people who you could deploy in a crisis, who already know where the vulnerable are and how to reach them – those were the kind of staff they used during 2009 swine flu to work closely with the NHS, but they have been lost,” Harrison said.

David Cameron, Nick Clegg and Andrew Lansley speaking with staff at Frimley Park hospital in 2011. Photograph: Reuters
“They took a perfectly well-functioning public health system and fractured it,” said Julie Hotchkiss, a PCT director with responsibility for emergency pandemic response who moved to York city council during the changes. She said it took her a year to work out where her infectious disease control nurses had gone. “No one knew and there was no one to ask.”
Dr Jeanelle de Gruchy, the president of the Association of Directors of Public Health, argues it was right for local authorities to have a key role in tackling health inequalities, which tend to relate to people’s living circumstances and socio-economic status. She regards the transfer of public health to local authorities as “incredibly important and positive”. But she adds: “It’s a very big job and the transition came at a time of cuts to the public sector, not just to local government, although those were huge.”
Lansley’s act also created an entirely new agency that has been at the centre of the response to the coronavirus outbreak: Public Health England. It was given two primary responsibilities: improving health and reducing inequalities by tackling “lifestyle” diseases, such as obesity; and protecting the public from infectious diseases and environmental hazards.
The HPA, which had previously taken a lead on infectious disease control, was folded into PHE. Martin McKee, a professor of European public health at the London School of Hygiene and Tropical Medicine, argues the result of all these new arrangements was “a hugely weakened and fragmented public health system with consequences writ large in Covid-19”.
The DHSC rejected the suggestion that the system was fragmented and that changes had affected the government’s ability to respond. Lord Lansley did too. He told the Guardian that an independent review of the public health changes from 2013 published by the the King’s Fund thinktank in January, “concluded that they were the right reforms, but were not supported subsequently by the right level of resources”. Combating health threats, such as pandemics, was “no more or less fragmented” after 2013, Lansley said, and the problem was not the new structures or moving public health to local government but money. “Our intention was for a real-terms increase in public health budgets alongside those for the NHS, but this was not followed through from 2015 onwards,” he said.
The ringfenced annual grant for public health from central government to local authorities – currently about £3.2bn – has been cut by a cumulative £850m in real terms since 2015-16, according to the King’s Fund review.
During his two-decade career in government, Scally had been involved in emergency responses for swine flu, foot and mouth, BSE, and the fuel crisis. For previous epidemics, he said, the government took “a public health approach; go in quick and hard, test, trace, isolate, throw everything at it”. But, he said, “the whole system was demolished” by Lansley’s changes, which led him to resign.
He then worked as an adviser for Labour’s former shadow health secretary, Andy Burnham, who is now the mayor of Greater Manchester. Burnham recalls Scally constantly warning him as Lansley’s bill was going through parliament that “we were losing pandemic preparedness”.
Testing time for Public Health England
No branch of government appears to have received more flak over its handling of the Covid-19 outbreak than Public Health England. The government’s chief scientific adviser, Sir Patrick Vallance, suggested it had failed to expand testing at the right moment. Its top executive has been criticised by leading public health experts, such as Prof Anthony Costello of University College London, for being “invisible”.
Even before the outbreak, the agency was a target of complaints from across the spectrum. Leftwing critics have accused PHE of failing to be tough enough in its role of promoting better health. The right has accused it of being the instrument of a nanny state with a bloated budget. PHE has had precious few political friends. But even those who might be natural allies – like Prof John Ashton, the former regional director of public health for north-west England – suggest it has “had a bad Covid war”.
Some of this might be down to bad luck. Its chief executive, Duncan Selbie, caught the virus along with key advisers in Westminster, and its director of health protection, Prof Paul Cosford, has cancer and has been self-isolating, although both have been working throughout.
However, there have also been structural challenges. The Lansley act created an agency that lacked independence from government, in contrast to its predecessor, the HPA. That has led to suspicions that some PHE decisions were politically influenced, such as the varying guidance on what kind of personal protective equipment (PPE) was needed for frontline staff treating Covid-19 patients. In late March, PHE said a lower specification of protective gowns than previously advised could be used, leading unions to accuse it of basing decisions on shortages of PPE, rather than evidence. This month, it downgraded the type of masks NHS workers should use “as a pragmatic approach for times of severe shortage”.
Greg Clark, the chair of the Commons science and technology select committee, accused PHE of choosing to “concentrate” tests in its own limited number of labs rather than expanding capacity rapidly by using university and private labs, as the Germans and South Koreans had done, even though the need for mass testing was “identifiable from the beginning”. PHE responded by blaming the DHSC, saying it was responsible for decisions on testing policy.
The DHSC spokesperson said: “Although Britain had a world-class pharmaceutical industry, it did not have the existing diagnostic base necessary to test hundreds of thousands of people each week for a new virus.” She said the government had more than doubled the capacity of NHS and PHE laboratories since early March, with more than 3m tests carried out by mid-May, and that anyone with symptoms could now book a test.
The government boasts that its new Test and Trace programme will mobilise an “army” of contact tracers. But in the two months leading up to 12 March, PHE’s team resembled no more than a small platoon. The Guardian has established it consisted of just 70 staff in its field services, 120 in local health protection teams, and 20 specially recruited clinical staff. In total, the contact tracing operation to manage the pandemic consisted of just 210 people.
Documents released on Friday by the government’s Scientific Advisory Group on Emergencies (Sage) suggest the contact-tracing operation initially only envisaged the need to deal with a handful of cases a week. Minutes from an 18 February meeting of the group said: “Currently PHE can cope with five new cases a week (requiring isolation of 800 contacts).” The minutes added: “Modelling suggests this capacity could be increased to 50 new cases a week (8,000 contact isolations) but this assumption needs to be stress-tested with PHE operational colleagues.”
Rather than ramp–up capacity, the government scientists instead agreed in the same meeting they would need data “to feed into trigger points for decisions on when the current monitoring and contact-tracing approach is no longer working”. The minutes added: “When there is sustained transmission in the UK, contact tracing will no longer be useful.”
PHE told the Sunday Telegraph that the reference to five cases a week was based on a modelling of how it would cope with imported cases of Covid-19 – and it was certain it had capacity to track and trace more cases at that time. “The model used an assumption of five importation events per week in the initial phase,” a PHE spokeswoman said. “This means five imported cases and subsequent cases that may arise as a consequence of those imported cases; the modelling considered the associated contacts for both. Modelling stated that the number of contacts could be managed by PHE.”
However, two days later, at another Sage meeting, the advisers acknowledged “individual cases could already have been missed” and again discussed when it would be appropriate to abandon the nascent operation. Appearing to acknowledge such a move would be controversial, the minutes said: “Any decision to discontinue contact tracing will generate a public reaction – which requires consideration with input from behavioural scientists.”
By the time community tracing was shelvedin mid–March, PHE had “contact traced” only 3,500 people who were likely to have been in close proximity with infected people on flights, cruises or other places where there were known outbreaks. Of those, only 3% tested positive for Covid-19 and were advised to self-isolate.
In other words, PHE had managed to identify and warn about 100 people with Covid-19 who might otherwise have spread the disease – a tiny fraction of the infected people. Vallance said there were 5,000 confirmed Covid cases when the community testing and tracing programme stopped, but epidemiologists at Imperial College London estimated 1.8 million people in Britain were infected by the end of March.
William Hanage, a professor of infectious disease epidemiology at Harvard University, said the numbers of PHE staff dedicated to contact tracing in Britain in the weeks leading up to mid-March was shocking. “I am sure that the people involved in this programme worked incredibly hard, and I have the utmost respect for them, tasked with doing this in the face of a global pandemic,” he said. “But it beggars belief to see these numbers held up as adequate.”
The elusive 100,000 target
On 2 April, three weeks after capacity had been overwhelmed and PHE had abandoned testing in the community, Hancock announced a five-pillar testing plan. He pledged to scale up the country’s testing capacity to reach a target of 100,000 tests a day by the end of the month.
But the architecture created in the postwar years to respond to pandemics was no longer standing. In the past, the Public Health Laboratories Service had been tasked with disease control, and with coordinating support and advice to the NHS and others. In 2003, Labour folded it into the HPA. Fifty PHLS labs that existed two decades ago have been merged with hospital labs or “consolidated” by successive governments to make efficiency savings. As of January this year, just eight laboratories remained under direct PHE control, along with 122 NHS labs in England.

Matt Hancock giving one of Downing Street’s daily coronavirus press briefings. Photograph: Pippa Fowles/10 Downing Street/AFP via Getty Images
Hancock expected hospital labs testing patients and staff and PHE to make up 25,000 of the ambitious 100,000 target. For the other 75,000 he turned to the private sector. Deloitte, one of the big four accountancy firms, was asked to set up a network of 50 drive-through rapid testing centres, and yet more private companies, such as Serco, Sodexo, Mitie and G4S, would operate and manage the day-to-day running of them.
A lab network to process the tests was also established. Deloitte was again given the coordinating role in the creation of new Lighthouse labs in Milton Keynes, Glasgow, Belfast and Cheshire and a further facility in Cambridge, with day-to-day running entrusted to a coalition of private and public partners, including universities and drug companies.
But Hancock’s 2 April announcement made no mention of one of the main purposes of testing: tracking or tracing.
The Guardian soon received reports from people trying to get tested of chaos at some sites, with results going astray, dangerously leaking swab samples arriving at labs, queues of more than three hours and symptomatic people being unable to book a test or told to make round trips of more than 100 miles to test centres. Many still report results taking seven to 10 days to arrive – too long to be useful for quarantine purposes – but the DHSC maintains that 97% of test results are obtained within 48 hours.
In the last week of April, the government changed its criteria for counting tests to include ones that had been dispatched, even if they had not been received, returned or processed. The date of 30 April came and Hancock missed his 100,000 target; the number of tests conducted that day was 81,611. But the next day, on 1 May, he appeared to smash it, as 122,347 tests were recorded in government data. The magic number had, by Hancock’s own admission, included nearly 30,000 postal tests sent out but not yet analysed. By 3 May the number was back down to 76,496, and the government would fail to meet its target for the next seven days, before getting back on track on 11 May.
For Chris Hopson, the chief executive of NHS Providers, which represents foundation trusts in England, Hancock’s single-minded focus on reaching an arbitrary number cost the country another precious month. “Too much of April was wasted by focusing on the 100,000 tests by 30 April target at the expense of other aspects of a clear strategy,” he said. “The testing strategy, if there was one, got hijacked on the basis of just meeting that target when there were lots of other things that needed to be done.”
Hopson said the saga also illustrates the danger of trying to control testing from the centre. “We need to be ready to do test, track and trace in every part of the country. That can only be done effectively with greater local control.”
Government reliance on private contractors follows dramatic changes to local councils and public services
by Felicity Lawrence, Juliette Garside, David Pegg, David Conn, Severin Carrell and Harry Davies
Sun 31 May 2020
FOR CHARTS AND LINKS
https://www.theguardian.com/world/2020/may/31/how-a-decade-of-privatisation-and-cuts-exposed-england-to-coronavirus
Every Thursday at 8pm, millions of Britons have opened their front doors or stood on balconies to applaud the NHS. The ritual has been a weekly expression of gratitude to medical workers, and national pride in a state-run health service said to be the envy of the world.
“Let’s not forget,” Boris Johnson said in early March, near the start of the coronavirus crisis, “we already have a fantastic NHS, fantastic testing systems and fantastic surveillance of the spread of disease.”
Yet those who have experienced the government’s emerging testing and tracing operations for Covid-19 have had limited contact with the NHS. Instead, Britons with symptoms are directed to a network of 50 drive-through testing centres, set up by management consultants at Deloitte.
Upon arrival, patients are marshalled not by NHS staff, but workers in hi-vis jackets supplied by outsourcing companies, such as Serco, G4S, Mitie and Sodexo. Those who cannot make the drive have received postal test kits, processed by the private diagnostics company Randox and delivered by Amazon.
When contact tracing to stop the spread of the virus finally moved up the agenda in late April, the health and social care secretary, Matt Hancock, said the job would be done with an as–yet unproven NHS app. The app has been developed by private firms for NHSX, the technology wing of the health service, which is also responsible for a Covid-19 government data operation involving tech companies Palantir, Faculty, Amazon, Google and Microsoft.
On Thursday the government finally launched its long-awaited NHS Test and Trace Service. But despite the name, many of the 25,000 contact tracers tracking those potentially exposed to Covid-19 and advising them to self-isolate will be working not for the NHS, but rather the outsourcing firms Serco and Sitel.
The government’s reliance on private contractors during the public health emergency comes after a decade of public sector reorganisation, marketisation and deep cuts to services and local government in England. The Guardian has interviewed dozens of public health directors, politicians, experts in infectious disease control, government scientific and political advisers, NHS leaders and emergency planners about the years leading up to the pandemic.
They described how an infrastructure that was once in place to respond to public health crises was fractured, and in some places demolished, by policies introduced by recent Conservative governments, with some changes going as far back as Labour’s years in power.
“The undermining of our responsiveness to a pandemic was one of my major concerns,” said Gabriel Scally, a professor of public health at the University of Bristol and a former regional director of public health in the NHS for almost 20 years. “There has been a destruction of the infrastructure that stops England coping with major emergencies. It absolutely explains why you’re now seeing private companies being brought into these functions.”
Councils left in the dark
Local authorities are the Cinderellas of government, their work often overlooked. But in the middle of a public health crisis, counties, districts and boroughs traditionally become the foot soldiers of national response. Few have been as badly hit as the east London borough of Newham, the local authority with the highest Covid-19 mortality rate in England and Wales.
Yet Newham’s director of public health, Jason Strelitz, was left in the dark at the start. He had no official notification that the virus had arrived in his area in mid-March, and only found out when he logged on to the government’s public coronavirus tracker web page to make his daily check on the declared numbers. Strelitz did not know who in Newham had Covid-19, where they had been tested, or which part of the borough they came from.
“We’re really concerned about the way national testing has been set up,” Strelitz said. “We still don’t have a clear picture of who is being tested in our area nor of the extent of community transmission in Newham.”
by Felicity Lawrence, Juliette Garside, David Pegg, David Conn, Severin Carrell and Harry Davies
Sun 31 May 2020
FOR CHARTS AND LINKS
https://www.theguardian.com/world/2020/may/31/how-a-decade-of-privatisation-and-cuts-exposed-england-to-coronavirus
Every Thursday at 8pm, millions of Britons have opened their front doors or stood on balconies to applaud the NHS. The ritual has been a weekly expression of gratitude to medical workers, and national pride in a state-run health service said to be the envy of the world.
“Let’s not forget,” Boris Johnson said in early March, near the start of the coronavirus crisis, “we already have a fantastic NHS, fantastic testing systems and fantastic surveillance of the spread of disease.”
Yet those who have experienced the government’s emerging testing and tracing operations for Covid-19 have had limited contact with the NHS. Instead, Britons with symptoms are directed to a network of 50 drive-through testing centres, set up by management consultants at Deloitte.
Upon arrival, patients are marshalled not by NHS staff, but workers in hi-vis jackets supplied by outsourcing companies, such as Serco, G4S, Mitie and Sodexo. Those who cannot make the drive have received postal test kits, processed by the private diagnostics company Randox and delivered by Amazon.
When contact tracing to stop the spread of the virus finally moved up the agenda in late April, the health and social care secretary, Matt Hancock, said the job would be done with an as–yet unproven NHS app. The app has been developed by private firms for NHSX, the technology wing of the health service, which is also responsible for a Covid-19 government data operation involving tech companies Palantir, Faculty, Amazon, Google and Microsoft.
On Thursday the government finally launched its long-awaited NHS Test and Trace Service. But despite the name, many of the 25,000 contact tracers tracking those potentially exposed to Covid-19 and advising them to self-isolate will be working not for the NHS, but rather the outsourcing firms Serco and Sitel.
The government’s reliance on private contractors during the public health emergency comes after a decade of public sector reorganisation, marketisation and deep cuts to services and local government in England. The Guardian has interviewed dozens of public health directors, politicians, experts in infectious disease control, government scientific and political advisers, NHS leaders and emergency planners about the years leading up to the pandemic.
They described how an infrastructure that was once in place to respond to public health crises was fractured, and in some places demolished, by policies introduced by recent Conservative governments, with some changes going as far back as Labour’s years in power.
“The undermining of our responsiveness to a pandemic was one of my major concerns,” said Gabriel Scally, a professor of public health at the University of Bristol and a former regional director of public health in the NHS for almost 20 years. “There has been a destruction of the infrastructure that stops England coping with major emergencies. It absolutely explains why you’re now seeing private companies being brought into these functions.”
Councils left in the dark
Local authorities are the Cinderellas of government, their work often overlooked. But in the middle of a public health crisis, counties, districts and boroughs traditionally become the foot soldiers of national response. Few have been as badly hit as the east London borough of Newham, the local authority with the highest Covid-19 mortality rate in England and Wales.
Yet Newham’s director of public health, Jason Strelitz, was left in the dark at the start. He had no official notification that the virus had arrived in his area in mid-March, and only found out when he logged on to the government’s public coronavirus tracker web page to make his daily check on the declared numbers. Strelitz did not know who in Newham had Covid-19, where they had been tested, or which part of the borough they came from.
“We’re really concerned about the way national testing has been set up,” Strelitz said. “We still don’t have a clear picture of who is being tested in our area nor of the extent of community transmission in Newham.”

Jason Strelitz at the Covid-19 hub for local authority action in Newham. Photograph: Graeme Robertson/The Guardian
In normal times, a Public Health England (PHE) representative would be expected to contact Strelitz’s environmental health teams if a case of a notifiable disease was found in the area that needed following up, enabling them to set to work tracing contacts and containing an outbreak. But the government had just abandoned community testing and tracing so local authorities were not being contacted at that point.
Newham is among the most deprived boroughs in the country. Like all the public health directors interviewed by the Guardian, Strelitz has deep knowledge of the characteristics of his patch that make its health inequalities so stark and its residents so vulnerable to the disease. About 30,000 people have been identified by the council as being at high risk – many of them over 70, living alone and isolated.
Even now, with large-scale community testing resumed, Strelitz said he was not receiving useful test data from the centralised, privately contracted operation created by Hancock. He also has concerns about the contact-tracing operation being set up.
In addition to the contact-tracing app, the government has once more turned to outsourcing companies, including Serco and Sitel, to recruit and train 25,000 contact tracers. Working on a salary just above minimum wage, the majority will have no medical training. Using scripts, they will contact those who have tested positive, trace people they have been in contact with, and advise them on how to isolate.
“Contact tracing is a sensitive issue – I’m not sure how well it can be done with a remote call centre with no understanding of people’s local context,” Strelitz said.
Dominic Harrison, the director of public health for Blackburn and Darwen, has similar concerns. Speaking earlier this month he said there was “a huge disconnect” between different branches of government, with some functions of the local public health system having been disabled in recent years.
“People like environmental health officers, community and neighbourhood teams, youth services workers – the people who you could deploy in a crisis, who already know where the vulnerable are and how to reach them – those were the kind of staff they used during 2009 swine flu to work closely with the NHS, but they have been lost,” Harrison said.

Council workers in Hull disinfect pavements and structures to guard against the transmission of coronavirus. Photograph: Lindsey Parnaby/AFP via Getty ImagesThe Labour leader of Nottingham city council, David Mellen, said Conservative ministers had spent so many years shrinking the state locally “they have forgotten what local authorities can do”. Nottingham has had its central government support grant cut by 80% since 2013 and, like many other councils, no longer has reserves for emergencies such as coronavirus. The Ministry of Housing, Communities and Local Government has made an emergency grant of £3.2bn to councils for Covid-19 costs, which the communities secretary, Robert Jenrick, has defended as fair and generous. Mellen disagrees. Nottingham, he said, had been given £19.8m as its share of the exceptional grant, but had already spent well over £12m extra on Covid-19 while losing at least £19m in revenue because of the lockdown.
A Department of Health and Social Care (DHSC) spokesperson did not dispute that cuts to central government grants could have had an impact on local public health networks. However, she pointed to the £3.2bn emergency funding for councils, which she said was in addition to an increase of £2.9bn in councils’ core spending power this year. “Protecting the public’s health is, and has always been, a priority for the UK government,” she said.
A decade of austerity
Next month, Britain will mark an anniversary many Conservative ministers would rather forget. Shortly after 12.30pm on 22 June 2010, George Osborne stepped up to the dispatch box as chancellor of the new coalition government and announced the longest and deepest period of cuts to public service spending since the second world war.
Ushering in a new age of austerity to a raucous Commons, Osborne outlined £81bn of cuts over five years. His aim was twofold: to eliminate the government’s budget deficit and to reduce its debt as a share of GDP. The emergency budget would, he said, bring the country back from the brink of ruin. “It pays for the past. It plans for the future. And it protects the most vulnerable in our society,” Osborne told MPs.
It was the prime minister, David Cameron, who had the previous year introduced the notion of “the age of irresponsibility giving way to the age of austerity”. He said he expected the public spending cuts would be permanent as the private and voluntary sectors stepped in to deliver public services better than the state could. Some government departments would be cut by a third and most public sector workers would have to accept a pay freeze.
Along with welfare, some of the most brutal reductions were imposed on local government in England as Osborne transferred the political risk of austerity to councils. Over the next decade, local authorities had 60% of their funding from central government cut, according to the Local Government Association. At the same time their ability to increase council tax, to try to replace the lost revenue, was capped. The cuts fell disproportionately on those authorities with the poorest populations.
Cameron promised he would “cut the deficit, not the NHS” and Osborne ringfenced its budget. It got cash increases, but these were less than 1% a year, and failed to keep pace with growing demand from an ageing population.
Approximately 32,000 overnight beds have been lost from hospitals in England in just over a decade, including some lost under Labour. Allyson Pollock, a professor of public health at Newcastle University, points out that the number of beds lost is roughly the same as the beds the NHS had to scramble to free up for Covid-19 patients.
When the coronavirus spread to Europe earlier this year, the UK ranked 24th among European countries for its numbers of critical care beds, with 6.6 per 100,000 population, compared with Germany, which topped the league with 29.2 per 100,000.
NHS fragmentation
Two years after Osborne’s announcement, with austerity beginning to bite, the then health secretary, Andrew Lansley, embarked on a complete market-oriented restructuring of the NHS. Despite Cameron’s pre-election promise that there would be no more pointless, disruptive top-down reorganisations, critics argue that Lansley’s 2012 Health and Social Care Act did just that.
Labour had done its fair share of subjecting the NHS to upheaval. Its programme of building new hospitals under the private finance initiative required other hospital and community health services to close, and shrank bed numbers to help cover the high annual fees to private companies. It accelerated changes brought in by the Conservatives to mimic a market, and created NHS trusts that could operate as semi-autonomous corporate bodies. By 2006, Labour’s reorganisations had created 152 primary care trusts (PCTs). Overarching priorities were set by regional strategic health authorities and the Department of Health.
But every area still had a Public Health Observatory, which included infectious disease control teams. Under government pandemic plans, each had to identify rapid response teams for testing and tracing, and these were activated during the swine flu outbreak in 2009.
Health authorities also had consultants in communicable disease control appointed at senior level on a par with NHS hospital consultants. An independent public body, the Health Protection Agency (HPA), provided specialist support on the threat of emerging diseases. There were critics of the structures, but in planning for emergencies there was, at least, a clear chain of command and control. “Labour started the process of fragmenting public health but it was at least still integrated with communicable disease control and the NHS,” Pollock said.
Lansley’s legislation did away with much of that. He abolished PCTs and strategic health authorities. Instead, existing public health structures were stripped out of the NHS and redistributed, along with their budgets and staff. In a dramatic shift, local authorities were given responsibility for public health for their areas, with larger ones being required to appoint a director of public health.
A Department of Health and Social Care (DHSC) spokesperson did not dispute that cuts to central government grants could have had an impact on local public health networks. However, she pointed to the £3.2bn emergency funding for councils, which she said was in addition to an increase of £2.9bn in councils’ core spending power this year. “Protecting the public’s health is, and has always been, a priority for the UK government,” she said.
A decade of austerity
Next month, Britain will mark an anniversary many Conservative ministers would rather forget. Shortly after 12.30pm on 22 June 2010, George Osborne stepped up to the dispatch box as chancellor of the new coalition government and announced the longest and deepest period of cuts to public service spending since the second world war.
Ushering in a new age of austerity to a raucous Commons, Osborne outlined £81bn of cuts over five years. His aim was twofold: to eliminate the government’s budget deficit and to reduce its debt as a share of GDP. The emergency budget would, he said, bring the country back from the brink of ruin. “It pays for the past. It plans for the future. And it protects the most vulnerable in our society,” Osborne told MPs.
It was the prime minister, David Cameron, who had the previous year introduced the notion of “the age of irresponsibility giving way to the age of austerity”. He said he expected the public spending cuts would be permanent as the private and voluntary sectors stepped in to deliver public services better than the state could. Some government departments would be cut by a third and most public sector workers would have to accept a pay freeze.
Along with welfare, some of the most brutal reductions were imposed on local government in England as Osborne transferred the political risk of austerity to councils. Over the next decade, local authorities had 60% of their funding from central government cut, according to the Local Government Association. At the same time their ability to increase council tax, to try to replace the lost revenue, was capped. The cuts fell disproportionately on those authorities with the poorest populations.
Cameron promised he would “cut the deficit, not the NHS” and Osborne ringfenced its budget. It got cash increases, but these were less than 1% a year, and failed to keep pace with growing demand from an ageing population.
Approximately 32,000 overnight beds have been lost from hospitals in England in just over a decade, including some lost under Labour. Allyson Pollock, a professor of public health at Newcastle University, points out that the number of beds lost is roughly the same as the beds the NHS had to scramble to free up for Covid-19 patients.
When the coronavirus spread to Europe earlier this year, the UK ranked 24th among European countries for its numbers of critical care beds, with 6.6 per 100,000 population, compared with Germany, which topped the league with 29.2 per 100,000.
NHS fragmentation
Two years after Osborne’s announcement, with austerity beginning to bite, the then health secretary, Andrew Lansley, embarked on a complete market-oriented restructuring of the NHS. Despite Cameron’s pre-election promise that there would be no more pointless, disruptive top-down reorganisations, critics argue that Lansley’s 2012 Health and Social Care Act did just that.
Labour had done its fair share of subjecting the NHS to upheaval. Its programme of building new hospitals under the private finance initiative required other hospital and community health services to close, and shrank bed numbers to help cover the high annual fees to private companies. It accelerated changes brought in by the Conservatives to mimic a market, and created NHS trusts that could operate as semi-autonomous corporate bodies. By 2006, Labour’s reorganisations had created 152 primary care trusts (PCTs). Overarching priorities were set by regional strategic health authorities and the Department of Health.
But every area still had a Public Health Observatory, which included infectious disease control teams. Under government pandemic plans, each had to identify rapid response teams for testing and tracing, and these were activated during the swine flu outbreak in 2009.
Health authorities also had consultants in communicable disease control appointed at senior level on a par with NHS hospital consultants. An independent public body, the Health Protection Agency (HPA), provided specialist support on the threat of emerging diseases. There were critics of the structures, but in planning for emergencies there was, at least, a clear chain of command and control. “Labour started the process of fragmenting public health but it was at least still integrated with communicable disease control and the NHS,” Pollock said.
Lansley’s legislation did away with much of that. He abolished PCTs and strategic health authorities. Instead, existing public health structures were stripped out of the NHS and redistributed, along with their budgets and staff. In a dramatic shift, local authorities were given responsibility for public health for their areas, with larger ones being required to appoint a director of public health.

David Cameron, Nick Clegg and Andrew Lansley speaking with staff at Frimley Park hospital in 2011. Photograph: Reuters
“They took a perfectly well-functioning public health system and fractured it,” said Julie Hotchkiss, a PCT director with responsibility for emergency pandemic response who moved to York city council during the changes. She said it took her a year to work out where her infectious disease control nurses had gone. “No one knew and there was no one to ask.”
Dr Jeanelle de Gruchy, the president of the Association of Directors of Public Health, argues it was right for local authorities to have a key role in tackling health inequalities, which tend to relate to people’s living circumstances and socio-economic status. She regards the transfer of public health to local authorities as “incredibly important and positive”. But she adds: “It’s a very big job and the transition came at a time of cuts to the public sector, not just to local government, although those were huge.”
Lansley’s act also created an entirely new agency that has been at the centre of the response to the coronavirus outbreak: Public Health England. It was given two primary responsibilities: improving health and reducing inequalities by tackling “lifestyle” diseases, such as obesity; and protecting the public from infectious diseases and environmental hazards.
The HPA, which had previously taken a lead on infectious disease control, was folded into PHE. Martin McKee, a professor of European public health at the London School of Hygiene and Tropical Medicine, argues the result of all these new arrangements was “a hugely weakened and fragmented public health system with consequences writ large in Covid-19”.
The DHSC rejected the suggestion that the system was fragmented and that changes had affected the government’s ability to respond. Lord Lansley did too. He told the Guardian that an independent review of the public health changes from 2013 published by the the King’s Fund thinktank in January, “concluded that they were the right reforms, but were not supported subsequently by the right level of resources”. Combating health threats, such as pandemics, was “no more or less fragmented” after 2013, Lansley said, and the problem was not the new structures or moving public health to local government but money. “Our intention was for a real-terms increase in public health budgets alongside those for the NHS, but this was not followed through from 2015 onwards,” he said.
The ringfenced annual grant for public health from central government to local authorities – currently about £3.2bn – has been cut by a cumulative £850m in real terms since 2015-16, according to the King’s Fund review.
During his two-decade career in government, Scally had been involved in emergency responses for swine flu, foot and mouth, BSE, and the fuel crisis. For previous epidemics, he said, the government took “a public health approach; go in quick and hard, test, trace, isolate, throw everything at it”. But, he said, “the whole system was demolished” by Lansley’s changes, which led him to resign.
He then worked as an adviser for Labour’s former shadow health secretary, Andy Burnham, who is now the mayor of Greater Manchester. Burnham recalls Scally constantly warning him as Lansley’s bill was going through parliament that “we were losing pandemic preparedness”.
Testing time for Public Health England
No branch of government appears to have received more flak over its handling of the Covid-19 outbreak than Public Health England. The government’s chief scientific adviser, Sir Patrick Vallance, suggested it had failed to expand testing at the right moment. Its top executive has been criticised by leading public health experts, such as Prof Anthony Costello of University College London, for being “invisible”.
Even before the outbreak, the agency was a target of complaints from across the spectrum. Leftwing critics have accused PHE of failing to be tough enough in its role of promoting better health. The right has accused it of being the instrument of a nanny state with a bloated budget. PHE has had precious few political friends. But even those who might be natural allies – like Prof John Ashton, the former regional director of public health for north-west England – suggest it has “had a bad Covid war”.
Some of this might be down to bad luck. Its chief executive, Duncan Selbie, caught the virus along with key advisers in Westminster, and its director of health protection, Prof Paul Cosford, has cancer and has been self-isolating, although both have been working throughout.
However, there have also been structural challenges. The Lansley act created an agency that lacked independence from government, in contrast to its predecessor, the HPA. That has led to suspicions that some PHE decisions were politically influenced, such as the varying guidance on what kind of personal protective equipment (PPE) was needed for frontline staff treating Covid-19 patients. In late March, PHE said a lower specification of protective gowns than previously advised could be used, leading unions to accuse it of basing decisions on shortages of PPE, rather than evidence. This month, it downgraded the type of masks NHS workers should use “as a pragmatic approach for times of severe shortage”.
Clinical staff wearing PPE as they care for a patient at the intensive care unit at Royal Papworth hospital in Cambridge. Photograph: Getty Images
PHE disputes that it was slow off the mark, and Selbie points out that it rolled out the details for its first diagnostic test in January, making it “the fastest deployment of a novel test in recent UK history”. It says the guidance on PPE has been misunderstood: it was offering a solution in the event of extreme shortages.
“Our track record speaks for itself,” a PHE spokesperson said. “During 2018-19 alone, we responded to more than 10,000 disease outbreaks and emergencies across England, including meningitis, measles, E coli and the first ever UK case of monkeypox. Our flu vaccination programme grows every year and cases of TB have fallen to the lowest level since records began.” They said that far from being invisible, Selbie had been at the coalface, helping to advise government on its decision-making.
The DHSC spokesperson cited a positive report by the International Association of National Public Health Institutes, which described PHE as a “strong, capable, coordinated, united and efficient public health agency”. The report only examined PHE and not the public health systems devolved to local authorities. The same report pointed out that “there is scope for greater clarity in the responsibilities of PHE’s local partners”.
In its defence, PHE has had to absorb disparate functions since its creation in 2013. And it too has been struck by austerity: a public health source said PHE’s operational budget sustained a 40% real-terms cut between 2013 and 2019.
It was PHE that initially had responsibility for testing, tracing and advising isolation for those who became infected. It was a huge and complicated task, but one the World Health Organization has made clear from the outset was the single most important thing countries could do to suppress the disease. The government’s decision to abandon large-scale testing and tracing on 12 March remains one of its most controversial decisions.
PHE says it reprioritised limited resources rather than abandoning tracing completely. “When the lockdown began, our contact-tracing resource was refocused on to complex outbreaks in care homes, prisons and immigration centres,” Selbie said. “The good news is, now that we have testing capacity in place and are working towards recovery, we can start mass contact tracing through the NHS test and trace programme.
“PHE’s contact tracing during the ‘‘contain’ phase of the pandemic bought several weeks of time for the government and the NHS to prepare for what was to come, and has undoubtedly saved lives,” he said.
PHE disputes that it was slow off the mark, and Selbie points out that it rolled out the details for its first diagnostic test in January, making it “the fastest deployment of a novel test in recent UK history”. It says the guidance on PPE has been misunderstood: it was offering a solution in the event of extreme shortages.
“Our track record speaks for itself,” a PHE spokesperson said. “During 2018-19 alone, we responded to more than 10,000 disease outbreaks and emergencies across England, including meningitis, measles, E coli and the first ever UK case of monkeypox. Our flu vaccination programme grows every year and cases of TB have fallen to the lowest level since records began.” They said that far from being invisible, Selbie had been at the coalface, helping to advise government on its decision-making.
The DHSC spokesperson cited a positive report by the International Association of National Public Health Institutes, which described PHE as a “strong, capable, coordinated, united and efficient public health agency”. The report only examined PHE and not the public health systems devolved to local authorities. The same report pointed out that “there is scope for greater clarity in the responsibilities of PHE’s local partners”.
In its defence, PHE has had to absorb disparate functions since its creation in 2013. And it too has been struck by austerity: a public health source said PHE’s operational budget sustained a 40% real-terms cut between 2013 and 2019.
It was PHE that initially had responsibility for testing, tracing and advising isolation for those who became infected. It was a huge and complicated task, but one the World Health Organization has made clear from the outset was the single most important thing countries could do to suppress the disease. The government’s decision to abandon large-scale testing and tracing on 12 March remains one of its most controversial decisions.
PHE says it reprioritised limited resources rather than abandoning tracing completely. “When the lockdown began, our contact-tracing resource was refocused on to complex outbreaks in care homes, prisons and immigration centres,” Selbie said. “The good news is, now that we have testing capacity in place and are working towards recovery, we can start mass contact tracing through the NHS test and trace programme.
“PHE’s contact tracing during the ‘‘contain’ phase of the pandemic bought several weeks of time for the government and the NHS to prepare for what was to come, and has undoubtedly saved lives,” he said.
Greg Clark, the chair of the Commons science and technology select committee, accused PHE of choosing to “concentrate” tests in its own limited number of labs rather than expanding capacity rapidly by using university and private labs, as the Germans and South Koreans had done, even though the need for mass testing was “identifiable from the beginning”. PHE responded by blaming the DHSC, saying it was responsible for decisions on testing policy.
The DHSC spokesperson said: “Although Britain had a world-class pharmaceutical industry, it did not have the existing diagnostic base necessary to test hundreds of thousands of people each week for a new virus.” She said the government had more than doubled the capacity of NHS and PHE laboratories since early March, with more than 3m tests carried out by mid-May, and that anyone with symptoms could now book a test.
The government boasts that its new Test and Trace programme will mobilise an “army” of contact tracers. But in the two months leading up to 12 March, PHE’s team resembled no more than a small platoon. The Guardian has established it consisted of just 70 staff in its field services, 120 in local health protection teams, and 20 specially recruited clinical staff. In total, the contact tracing operation to manage the pandemic consisted of just 210 people.
Documents released on Friday by the government’s Scientific Advisory Group on Emergencies (Sage) suggest the contact-tracing operation initially only envisaged the need to deal with a handful of cases a week. Minutes from an 18 February meeting of the group said: “Currently PHE can cope with five new cases a week (requiring isolation of 800 contacts).” The minutes added: “Modelling suggests this capacity could be increased to 50 new cases a week (8,000 contact isolations) but this assumption needs to be stress-tested with PHE operational colleagues.”
Rather than ramp–up capacity, the government scientists instead agreed in the same meeting they would need data “to feed into trigger points for decisions on when the current monitoring and contact-tracing approach is no longer working”. The minutes added: “When there is sustained transmission in the UK, contact tracing will no longer be useful.”
PHE told the Sunday Telegraph that the reference to five cases a week was based on a modelling of how it would cope with imported cases of Covid-19 – and it was certain it had capacity to track and trace more cases at that time. “The model used an assumption of five importation events per week in the initial phase,” a PHE spokeswoman said. “This means five imported cases and subsequent cases that may arise as a consequence of those imported cases; the modelling considered the associated contacts for both. Modelling stated that the number of contacts could be managed by PHE.”
However, two days later, at another Sage meeting, the advisers acknowledged “individual cases could already have been missed” and again discussed when it would be appropriate to abandon the nascent operation. Appearing to acknowledge such a move would be controversial, the minutes said: “Any decision to discontinue contact tracing will generate a public reaction – which requires consideration with input from behavioural scientists.”
By the time community tracing was shelvedin mid–March, PHE had “contact traced” only 3,500 people who were likely to have been in close proximity with infected people on flights, cruises or other places where there were known outbreaks. Of those, only 3% tested positive for Covid-19 and were advised to self-isolate.
In other words, PHE had managed to identify and warn about 100 people with Covid-19 who might otherwise have spread the disease – a tiny fraction of the infected people. Vallance said there were 5,000 confirmed Covid cases when the community testing and tracing programme stopped, but epidemiologists at Imperial College London estimated 1.8 million people in Britain were infected by the end of March.
William Hanage, a professor of infectious disease epidemiology at Harvard University, said the numbers of PHE staff dedicated to contact tracing in Britain in the weeks leading up to mid-March was shocking. “I am sure that the people involved in this programme worked incredibly hard, and I have the utmost respect for them, tasked with doing this in the face of a global pandemic,” he said. “But it beggars belief to see these numbers held up as adequate.”
The elusive 100,000 target
On 2 April, three weeks after capacity had been overwhelmed and PHE had abandoned testing in the community, Hancock announced a five-pillar testing plan. He pledged to scale up the country’s testing capacity to reach a target of 100,000 tests a day by the end of the month.
But the architecture created in the postwar years to respond to pandemics was no longer standing. In the past, the Public Health Laboratories Service had been tasked with disease control, and with coordinating support and advice to the NHS and others. In 2003, Labour folded it into the HPA. Fifty PHLS labs that existed two decades ago have been merged with hospital labs or “consolidated” by successive governments to make efficiency savings. As of January this year, just eight laboratories remained under direct PHE control, along with 122 NHS labs in England.

Matt Hancock giving one of Downing Street’s daily coronavirus press briefings. Photograph: Pippa Fowles/10 Downing Street/AFP via Getty Images
Hancock expected hospital labs testing patients and staff and PHE to make up 25,000 of the ambitious 100,000 target. For the other 75,000 he turned to the private sector. Deloitte, one of the big four accountancy firms, was asked to set up a network of 50 drive-through rapid testing centres, and yet more private companies, such as Serco, Sodexo, Mitie and G4S, would operate and manage the day-to-day running of them.
A lab network to process the tests was also established. Deloitte was again given the coordinating role in the creation of new Lighthouse labs in Milton Keynes, Glasgow, Belfast and Cheshire and a further facility in Cambridge, with day-to-day running entrusted to a coalition of private and public partners, including universities and drug companies.
But Hancock’s 2 April announcement made no mention of one of the main purposes of testing: tracking or tracing.
The Guardian soon received reports from people trying to get tested of chaos at some sites, with results going astray, dangerously leaking swab samples arriving at labs, queues of more than three hours and symptomatic people being unable to book a test or told to make round trips of more than 100 miles to test centres. Many still report results taking seven to 10 days to arrive – too long to be useful for quarantine purposes – but the DHSC maintains that 97% of test results are obtained within 48 hours.
In the last week of April, the government changed its criteria for counting tests to include ones that had been dispatched, even if they had not been received, returned or processed. The date of 30 April came and Hancock missed his 100,000 target; the number of tests conducted that day was 81,611. But the next day, on 1 May, he appeared to smash it, as 122,347 tests were recorded in government data. The magic number had, by Hancock’s own admission, included nearly 30,000 postal tests sent out but not yet analysed. By 3 May the number was back down to 76,496, and the government would fail to meet its target for the next seven days, before getting back on track on 11 May.
For Chris Hopson, the chief executive of NHS Providers, which represents foundation trusts in England, Hancock’s single-minded focus on reaching an arbitrary number cost the country another precious month. “Too much of April was wasted by focusing on the 100,000 tests by 30 April target at the expense of other aspects of a clear strategy,” he said. “The testing strategy, if there was one, got hijacked on the basis of just meeting that target when there were lots of other things that needed to be done.”
Hopson said the saga also illustrates the danger of trying to control testing from the centre. “We need to be ready to do test, track and trace in every part of the country. That can only be done effectively with greater local control.”