Trump’s Deregulatory Bonanza Leaves Workers Unsafe on the Job
Earlier this month, the Trump Department of Labor (DOL) unveiled a sweeping deregulation plan targeting a range of labor protections, including key workplace safety rules. Officials framed the effort as “a push to put the American worker first,” an Orwellian spin on policies that make it easier for employers to endanger their employees and harder for workers to hold them accountable. By weakening rules that protect health, safety, and dignity on the job, the plan is clearly designed to cut costs for employers by shifting risk and harm onto workers.
Undermining OSHA’s General Duty Clause
One of the most significant changes is a proposal to restrict how the Occupational Safety and Health Administration (OSHA) enforces its General Duty Clause, which requires workplaces to be “free from recognized hazards that are causing or are likely to cause death or serious physical harm.” The clause functions as a key backstop for OSHA enforcement, empowering the agency to address serious workplace hazards that fall outside the scope of more targeted regulations. The Trump regime wants to limit enforcement of this clause in industries it deems “inherently risky,” such as sports and entertainment, opening the door for employers in other industries to make similar arguments. The proposal echoes Brett Kavanaugh’s 2014 dissent in SeaWorld of Florida v. Perez, where he opposed applying the General Duty Clause after an amusement park trainer’s death, arguing that the risks were inherent to the job.
The COVID-19 pandemic has already shown how employers exploit the notion of “inherent risk” to avoid investing in meaningful prevention and safety measures. The new proposal solicits input on what should be considered inherently risky, opening the door to intense lobbying by industry heavyweights eager to avoid investing in worker safety.
Because no regulation can specify every possible hazard, the General Duty Clause is one of OSHA’s most important enforcement tools. Without the clause’s broad protections, OSHA would be far less able to respond to emerging hazards or to hold employers accountable for known dangers that fall between the gaps of existing rules. Weakening it would undermine worker protections across industries, though the proposal is likely to face legal challenges. Employers already have broad discretion to define what is “essential” to a job and to set workplace norms, especially in non-unionized settings. This tactic mirrors how some employers skirt their obligations under the Americans with Disabilities Act by insisting, for example, that lifting 50 pounds is an essential function of an office job, or by declaring that tasks incompatible with accommodations are non-negotiable rather than finding creative ways to make work safer and more accessible.
Downplaying the Ongoing Toll of COVID-19
Speaking of COVID-19, the administration also plans to formally remove COVID-19 emergency reporting rules for healthcare settings from federal regulations and end OSHA’s separate system for tracking COVID-related fatalities and hospitalizations. They would revert to the general reporting standards for workplace hazards, under which employers are only required to report hospitalizations if they occur within 24 hours of the workplace exposure. Reverting to OSHA’s baseline reporting standard would effectively erase most workplace-related COVID cases from the record, since most COVID-related hospitalizations happen several days or even weeks after exposure.
Officials argue that the emergency workplace reporting rules are no longer necessary, equating COVID-19 with seasonal flu and other common diseases. But while influenza and other respiratory illnesses are serious and deserve stronger prevention measures than they currently receive, COVID-19 remains more deadly(especially for seniors), more transmissible, and more likely to cause long-term disability. It continues to kill thousands of people in the US each year. It leaves many more with Long COVID, a devastating collection of chronic symptoms following an acute infection that can impair multiple organ systems. COVID-19 is also associated with increased risks of cardiac events, strokes, and other serious health complications months or even years after infection.
Ending separate COVID-19 reporting undermines our ability to track how and where the virus is spreading in workplaces, particularly in healthcare settings where vulnerable patients may be at risk of exposure. Accurate, up-to-date information about COVID-19 in medical facilities is essential to keeping those settings safe, protecting access to care, and preventing outbreaks that disproportionately harm people already at risk. Rather than abandoning COVID-specific reporting, OSHA should strengthen its surveillance of all infectious hazards and adopt a broader, prevention-focused approach to keeping workers and the public safe.
Ignoring Musculoskeletal Injuries
Another proposal would roll back employer reporting requirements for musculoskeletal disorders (MSDs), even though these injuries are among the most common and costly workplace hazards. MSDs are not conditions workers simply develop on their own — they are injuries caused or aggravated by poor workplace ergonomics, repetitive motions, heavy lifting, and other physically demanding tasks performed without proper protections.
MSDs are especially widespread in warehousing and transportation, and are the number one cause of injuries among warehousing and “last-mile delivery” workers. These are jobs where inadequate equipment and unsafe work practices routinely put workers at risk. OSHA currently has no dedicated ergonomics standard and relies on the General Duty Clause to cite employers for hazardous conditions. Congress blocked OSHA from issuing an ergonomics rule in 2001 and barred the agency from adopting another similar rule without new explicit legislation. However, dedicated tracking could improve the data necessary for lawmakers to revisit this issue. Eliminating dedicated MSD reporting threatens to further delay progress on one of the most common workplace health and safety issues.
Delaying Heat Protections
Outside of the deregulation plan, there are other indications of the White House’s contempt for worker safety. Amid rising temperatures and a surge in heat-related workplace deaths, the Trump Labor Department has shown little urgency in finalizing OSHA’s proposed heat protections. Under the Biden administration, OSHA drafted a rule with basic safeguards, including access to water, shaded or cooled break areas, and acclimatization protocols when temperatures reach 80°F. At 90°F, the rule would entitle workers to 15-minute breaks every two hours. These modest protections were intended to reduce heat-related illnesses and save lives.
Yet progress has slowed, and the administration’s choice to nominate David Keeling to lead OSHA underscores its disregard for workers’ safety. Keeling previously oversaw health and safety at Amazon and UPS, two companies widely criticized for failing to protect workers from dangerous heat. His nomination reflects the Trump administration’s anti-worker agenda and raises serious concerns about the future of OSHA’s heat protections and other workplace safety initiatives.
At the same time, the administration has already gutted other heat-related efforts, including firing staff at the National Institute for Occupational Safety and Healthwho were focused on protecting farm and construction workers from deadly heat. OSHA’s proposed heat rule has not yet been formally withdrawn, and the agency’s National Emphasis Program for Outdoor and Indoor Heat-Related Hazards remains in place through April 2026. But without strong leadership and urgency, these protections risk being delayed, weakened, or quietly abandoned, leaving workers exposed to an increasingly deadly threat.
The Trump Department of Labor’s deregulation push is not about putting workers first. It shields employers from accountability, even when their actions lead to injury, illness, or death. From weakening the General Duty Clause to slow-rolling data collection and protections against heat stress and long-term injuries, the Trump regime’s deregulatory push signals a willingness to sacrifice workers’ health and lives for the sake of corporate profit, as if efficiency requires treating workers as though they’re expendable. This is not about clearing away outdated or unnecessary rules. It chips away at the very principle that workers are entitled to safe and dignified working conditions. It signals to employers that cutting corners is acceptable and that the government will look the other way while workers are exploited and then discarded.
The government has shown it is prepared to gut key safety requirements to boost corporate profits. But workplace protections exist because workers fought for them. They are not favors from employers or politicians, but rights that workers won through struggle and sacrifice. The Trump Labor Department’s agenda makes it clear that those rights can be taken away if the working class becomes complacent. Protecting workers’ health, safety, and dignity depends on holding employers and the government accountable and rejecting the notion that preventable harm is simply part of the job.
This first appeared on CEPR.
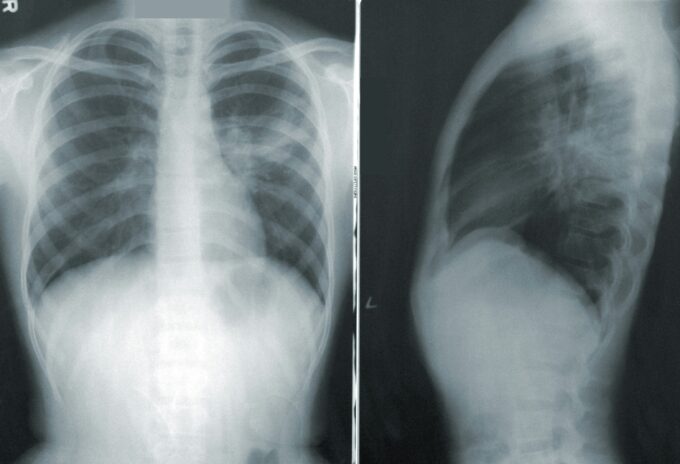
Image by CDC.
In 1976, thousands of patriotic veterans of the American Legion gathered in Philadelphia for the nation’s Bicentennial Celebration. It should have been a festive occasion, but it soon proved deadly. Nearly 300 attendees contracted an unfamiliar form of pneumonia that left them coughing, sneezing and in many cases, struggling to breathe.
In the end, nearly two dozen of those sufferers died in one of the worst infectious disease outbreaks in the city’s modern history.
An enterprising young Philadelphia Inquirer reporter was on hand to report on the outbreak but no one at the paper knew what to call the illness. After calls to local public health officials proved fruitless, the paper’s editor struck upon a name for the illness: “Legionnaires’ Disease.” It stuck.
Legionnaires’ Disease is said to be fairly rare, with less than 10,000 full-blown cases reported annually. But experts believe the real number may be closer to 70,000, or even higher. That would make Legionnaire’s the leading waterborne-borne infectious disease in the country – but you’d hardly know it from the dearth of attention it’s received.
While about 10% of those that contract the illness die from it, a large number only suffer moderate flu-like symptoms — “Pontiac Fever” — that do not require hospitalization. That’s one reason the illness still exists largely under the radar.
Legionnaire’s is also unique – and seemingly less threatening — because it is not contagious from one person to the other. Individuals are exposed by inhaling bacteria that grows in stagnant water through the air or soil.
Hospitals, spas, gyms and hotels – sometimes their hot tubs and showers, but just as often their HVAC systems — are the most common breeding grounds.
The incidence of Legionnaire’s Disease grew nine times between 2000 and 2017. 2018 saw the highest number of Legionnaires cases in over two decades. There’s some evidence that the incidence rate might have slowed somewhat since then, but sporadic outbreaks spiked in 2024. Public health specialists remain largely baffled by the overall trend — and in the absence of aggressive federal and state prevention efforts, are increasingly worried about what the future may hold.
Origins and causes
It’s generally agreed that America’s decaying infrastructure, coupled with the nation’s steadily ”graying” population. is a major spur to the disease. As older buildings continue to deteriorate, their piping systems become corrupted with large build-ups of water in temperature ranges that facilitate the growth of Legionella. And older Americans, those over 50-years-old, with weaker immune systems, including retirees living in congested facilities, are much more likely to find themselves vulnerable to sudden attack – and death.
These conditions were clearly in play in 1976 when large numbers of seniors attending the same event and staying in the same hotels were struck with the disease. With the US population still aging rapidly, and despite recent efforts to tackle big infrastructure problems (bridges, roads, etc.) legislatively, public and commercial buildings are continuing to deteriorate, so the risk of further Legionella spikes remains.
Ethnicity – or “systemic racism”– is another factor. Arguably, the most dilapidated housing and unsafe water systems are located in low-income minority-dominated neighborhoods. Residents there suffer other disease problems, including asthma, diabetes and poor sleep, disproportionately. Several studies have documented substantially higher incidence rates for Legionnaires disease among minority residents of dense, multi-family inner-city neighborhoods.
Minority families not only have a greater likelihood for Legionella in their homes, they also have fewer resources to spend on costly water testing and filtration systems.
Has “Going Green” Increased the Risk?
One of the ironies – though little discussed – is that modern “green” buildings, which tend to conserve water at moderately warm temperatures, may also be causing the number of Legionella cases to rise. This trend is the opposite of the decay factors associated with dilapidated buildings and infrastructure.
Green-certified or LEED buildings, under the banner of the “One Living Building Challenge,” are designed to be independent of water facilities. These buildings use water-saving equipment to reduce water consumption, in addition to rainwater collection, reservoirs, and other methods. LEED-certified green buildings typically save 20–50% of drinking water, for example. However, such design configurations pose unique challenges and corresponding public health problems. Water-saving measures, by their nature, increase stagnation and overall water age. The problem is found at both the municipal level – the primary water distribution system – and at the building level.
Another potential problem with green-building design is lowering the temperature of the water in the name of “energy-saving.” According to one authoritative study: “Lowering the temperature of water heater outlets could increase the possibility of Legionella detection and the degree of contamination of faucets significantly. Moreover, turning off the recirculation system at night causes stagnation for up to 8 hours or longer. Even in thermal insulation systems, water reaches the desired temperature for Legionella growth during such a long arrest period.”
Other common green-building measures, including the use of heat pumps and solar water heaters, can also lead to water temperatures beneficial for Legionella growth. One authoritative study found that the added storage incurred by a solar water heater in a net zero energy home increased the hot-water age from 1 day to as much as 3 days; on cloudy days, a preheated tank contained water squarely within the optimal temperature range for Legionella growth, the study found.
The upshot? When cities in concentrated urban areas go “green,” they may be inadvertently increasing the risk of generating Legionella growth across an entire swath of new environmentally-sustainable residential units.
Legionella and COVID-19
The massive shutdown of public buildings and commercial facilities, followed by their sudden re-opening after the COVID-19 pandemic has created another potential breeding ground for Legionnaire disease outbreaks. It turns out that the two diseases, in their earliest stages, often resemble each other. Both often start with a fever and a cough, though there may be additional gastrointestinal disturbances with Legionnaires.
Moreover, research strongly suggests that the two diseases are frequently “co-occurring,” which means that one can mask the other, disguising the heightened mortality risk. Increased screening for COVID-19 alone hasn’t necessarily made it easier to detect Legionnaires, which despite heightened risk-awareness among public health professionals, remains mysterious and difficult to predict – and remediate – with precision.
While some national surveillance data has failed to detect a significant spike in Legionella cases in the immediate post-pandemic period, regional and state-level data strongly suggests otherwise. Many of these cases were concentrated in the Northeast, especially New York, or in the Midwest.
For example, in 2021 Michigan’s Health Department recorded a nearly 600% increase in Legionella cases compared to 2020 and a 261% increase from 2019. Similarly, the Chicago government has reported an increase of three times from the cases reported for 2020 and 2019. In 2025 alone, severe outbreaks have been recorded in Las Vegas, NV, Columbus, OH, and most recently, Baltimore, MD.
Maryland has been especially hard hit. Since July 2024, 15 government buildings across the state have tested positive for high levels of Legionella, with the bacteria showing up in July, November, December, January and February — at times recurring in the same buildings – despite treatment.
Remediation efforts hampered
Defective water systems are clearly one root cause of Legionnaires; these water systems, once identified, need to be flushed out – or replaced. Since 2017, the Centers for Medicare & Medicaid Services (CMS) has mandated that health care facilities have water management plans in place to deter the growth of Legionella, the bacteria behind the disease.
However, even good water management plans are not necessarily effective, research shows. In Missouri in 2017, a study of 61 hospitals, nursing homes and hotels in the state found 7 to be infected with Legionella. But all 7 had water management plans in place.
“Legionella finds places within large complex water systems to hide,” says Jonathan Garoutte, administrator of the Missouri health department’s section for environmental public health.
Some observers note that the new CMS guidance, while useful in theory, also lacks enforcement teeth. In fact, many private health care providers have refused to comply, citing the exorbitant costs, and forcing CMS to back down.
In 2020, the agency said it would not formally require health care facilities to test for Legionella or other waterborne pathogens. “Testing protocols are at the discretion of the provider,” the directive said.
In response some public health officials are pushing back and demanding even stronger guidelines.
In a report released in August 2019, the prestigious National Academies of Sciences, Engineering and Medicine (NASEM) called for sweeping national protocols to reduce the threat from Legionnaire’s Disease. These included:
Extending the scope and standards of the federal Safe Drinking Water Act (SDWA) beyond public water supplies to include all public and private buildings vulnerable to Legionella growth
Requiring all public buildings to have a formal water management plan subject to regular inspections and fines for non-compliance.
Mandatory monitoring of water temperatures in all buildings, public and private, including “green” buildings, to deter Legionella growth.
New recommended codes and guidelines for water heating and air cooling systems manufactured in private industry.
Expanding communications to private homeowners on the need to flush their shower and bathroom taps to prevent the build-up of stagnant water.
The NASEM report, the first of its kind, is suggestive of just how seriously federal health authorities now take the potential threat from Legionnaire’s Disease.
In a 2022 op-ed, three health scientists with the Bloomberg School of Public Health called on federal health authorities to take even stronger measures. Noting the ethical duty to protect vulnerable at-risk groups, the authors urged the CDC local health departments and HUD to compel stronger housing inspection guidelines in low-income neighborhoods and to provide dedicated financial and technical support to assess the potential for Legionella poisoning alongside of other notorious home hazards (e.g. lead poisoning).
“The public health community needs to go outside the box to help ensure healthy drinking water,” the authors urged.
Some sectors of private industry are likely to take new steps to comply with these recommended guidelines, if only to reduce the threat of legal liability from a future outbreak. But mandating a tougher enforcement regime nationally may still be years away. The Biden administration, despite growing alarm from public health specialists., largely ignored the brewing Legionella crisis. And his successor, who is decimating federal health agencies, can’t be counted on to address the crisis, either. It’s not even on his radar screen.
Experts say we should expect an uptick in severe Legionella outbreaks in the coming years, some of them fatal, most of which could be prevented with greater policy attention and a renewed commitment of budget resources.
Conclusion
A half century ago, Legionnaires Disease came out of nowhere to shock the public health establishment into recognition of new waterborne infection threats. And yet despite the passage of time, much about the disease remains mysterious. Because its scale is still relatively low, Legionnaires has not received the priority attention it deserves, given the severe mortality risk, if not treated promptly. The continuing decay of old housing infrastructure, the ongoing “graying “ of the US population and the perverse and paradoxical challenge posed by popular “green” building initiatives provide good reason to be concerned about the possibility of future Legionella disease outbreaks. But for diverse reasons, neither of the two parties has chosen to focus federal and state resources on Legionella as a looming public health threat.
And the global prognosis could well be much worse. Legionella regulations and standards in developed countries were created fairly early, with well-established national and state-level surveillance systems already in place. That’s less true in developing countries, such as China, which has yet to list Legionnaires’ disease as a national infection threat. Without ongoing surveillance, and limited public awareness, the risk of transmission escalates. It’s also less true in some major Western nations. In 2024, as in the US, there were severe outbreaks in Australia, New Zealand and Italy. Legionnaires, like COVID, is no respecter of national boundaries.
Surveillance systems need not be technologically advanced to be effective, experts say. In fact, there are multiple low-cost approaches available to detect and quantify Legionella, but there must be the political will to overcome entrenched private interests, bureaucratic obstacles and even ideological resistance (from sustainability advocates) to authorize improved analysis of the sources of Legionella infections.
There is some good news about Legionnaires. Effective treatment is readily available. The two most potent classes of antibiotic available are the macrolides (azithromycin), and the quinolones (ciprofloxacin, levofloxacin, moxifloxacin and gemifloxacin). But sufferers need to obtain the medicine quickly, or the risk of death, especially for those with pre-existing conditions, increases rapidly. That’s especially true in the developing world, where obtaining ready access to expensive medicines at affordable prices – assuming a prompt screening and proper hospital care – is likely to remain a challenge for some time. But a lack of health equity is a persistent US problem, too. Sadly, it may just take another Legionella outbreak on the scale of the 1976 event to finally get policy-makers to focus.

No comments:
Post a Comment