A decades-long study finds that many prostate cancer patients can delay aggressive treatments and instead receive "active surveillance."
By Nicoletta Lanese published about 6 hours ago
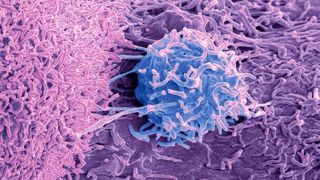
Many patients with prostate cancer can opt for "active surveillance" instead of seeking aggressive treatment right away.
(Image credit: STEVE GSCHMEISSNER/SCIENCE PHOTO LIBRARY via Getty Images)
Many men with prostate cancer can delay or skip harsh treatments, such as surgery or radiation, without undermining their chances of survival, a decades-long study finds.
Instead, they can have their cancer "actively monitored" following diagnosis, rather than having their prostate removed or exposed to high-energy radiation. Such treatments can cause long-lasting side effects, such as urinary leakage, erectile dysfunction and other problems with urinary, bowel and sexual function.
"The good news is that if you're diagnosed with prostate cancer, don't panic, and take your time to make a decision" about how to proceed, lead study author Dr. Freddie Hamdy(opens in new tab), professor of surgery and urology at the University of Oxford, told CNN(opens in new tab). Crucially, this advice only extends to people with low- or intermediate-risk prostate cancer — those with high-risk cancer still need prompt and aggressive treatment, he said.
The new study, published Saturday (March 11) in the New England Journal of Medicine(opens in new tab), included more than 1,600 men in the U.K. who'd been diagnosed with prostate cancer and ranged from 50 to 69 years old at the start of the trial. These patients were randomly divided into three groups that received different cancer treatments: one-third had their prostates removed, one-third got radiation in combination with a short-term hormone blocking treatment, and one-third underwent active monitoring, now commonly called "active surveillance."
During the study, which began in 1999, active surveillance meant regularly measuring levels of a specific protein in the patients' blood. Levels of this protein, called prostate-specific antigen (PSA), tend to rise as prostate cancer progresses. Today, active surveillance can involve additional tests, such as magnetic resonance imaging (MRI) scans of the prostate and genetic testing, Dr. Oliver Sartor(opens in new tab), medical director of the Tulane Cancer Center, wrote in a commentary(opens in new tab) of the research.
The researchers monitored each participant for 11 to 21 years post-diagnosis, and found that all the patients had a similarly low risk of death, regardless of the treatment they'd received. Overall, 45 participants, or 2.7%, died of prostate cancer. This included 12 people (2.2%) in the surgery group; 16 people (2.9%) in the radiation group; and 17 people (3.1%) in the active-monitoring group; these small differences are not considered statistically significant.
During the roughly 15-year follow-up period, about 330 men in the monitoring group, or 60%, eventually had either surgery or radiation treatment. But waiting to get treatment didn't seem to impact their risk of death. Furthermore, 133 people in the monitoring group never had surgery, radiation or hormone blocking therapy and still survived.
At 15 years post-diagnosis, cancer had metastasized, or spread, in 9.4% of the active-monitoring group, 4.7% of the surgery group and 5% of the radiation group. However, the monitoring group may have fared better if the study had been conducted with today's methods of surveillance, Dr. Stacy Loeb(opens in new tab), a prostate cancer specialist at NYU Langone Health who was not involved in the research, told The Associated Press(opens in new tab). "We have more ways now to help catch that the disease is progressing before it spreads," Loeb said.
It's key to note that "the vast majority of the trial patients were at low risk or favorable intermediate risk and would today be considered appropriate candidates for active surveillance," and only a small fraction of study participants would be considered high-risk and in need of immediate treatment, Sartor wrote in his commentary.
In general, high-risk prostate cancer diagnoses account for only 15% of cases — so most of the time, prostate cancer is of low- to intermediate-risk, CNN reported. For low-risk patients, the potential risks and benefits of surgery and radiation should be carefully weighed, since "more aggressive therapy can result in more harm than good," the study authors concluded.
Many men with prostate cancer can delay or skip harsh treatments, such as surgery or radiation, without undermining their chances of survival, a decades-long study finds.
Instead, they can have their cancer "actively monitored" following diagnosis, rather than having their prostate removed or exposed to high-energy radiation. Such treatments can cause long-lasting side effects, such as urinary leakage, erectile dysfunction and other problems with urinary, bowel and sexual function.
"The good news is that if you're diagnosed with prostate cancer, don't panic, and take your time to make a decision" about how to proceed, lead study author Dr. Freddie Hamdy(opens in new tab), professor of surgery and urology at the University of Oxford, told CNN(opens in new tab). Crucially, this advice only extends to people with low- or intermediate-risk prostate cancer — those with high-risk cancer still need prompt and aggressive treatment, he said.
The new study, published Saturday (March 11) in the New England Journal of Medicine(opens in new tab), included more than 1,600 men in the U.K. who'd been diagnosed with prostate cancer and ranged from 50 to 69 years old at the start of the trial. These patients were randomly divided into three groups that received different cancer treatments: one-third had their prostates removed, one-third got radiation in combination with a short-term hormone blocking treatment, and one-third underwent active monitoring, now commonly called "active surveillance."
During the study, which began in 1999, active surveillance meant regularly measuring levels of a specific protein in the patients' blood. Levels of this protein, called prostate-specific antigen (PSA), tend to rise as prostate cancer progresses. Today, active surveillance can involve additional tests, such as magnetic resonance imaging (MRI) scans of the prostate and genetic testing, Dr. Oliver Sartor(opens in new tab), medical director of the Tulane Cancer Center, wrote in a commentary(opens in new tab) of the research.
The researchers monitored each participant for 11 to 21 years post-diagnosis, and found that all the patients had a similarly low risk of death, regardless of the treatment they'd received. Overall, 45 participants, or 2.7%, died of prostate cancer. This included 12 people (2.2%) in the surgery group; 16 people (2.9%) in the radiation group; and 17 people (3.1%) in the active-monitoring group; these small differences are not considered statistically significant.
During the roughly 15-year follow-up period, about 330 men in the monitoring group, or 60%, eventually had either surgery or radiation treatment. But waiting to get treatment didn't seem to impact their risk of death. Furthermore, 133 people in the monitoring group never had surgery, radiation or hormone blocking therapy and still survived.
At 15 years post-diagnosis, cancer had metastasized, or spread, in 9.4% of the active-monitoring group, 4.7% of the surgery group and 5% of the radiation group. However, the monitoring group may have fared better if the study had been conducted with today's methods of surveillance, Dr. Stacy Loeb(opens in new tab), a prostate cancer specialist at NYU Langone Health who was not involved in the research, told The Associated Press(opens in new tab). "We have more ways now to help catch that the disease is progressing before it spreads," Loeb said.
It's key to note that "the vast majority of the trial patients were at low risk or favorable intermediate risk and would today be considered appropriate candidates for active surveillance," and only a small fraction of study participants would be considered high-risk and in need of immediate treatment, Sartor wrote in his commentary.
In general, high-risk prostate cancer diagnoses account for only 15% of cases — so most of the time, prostate cancer is of low- to intermediate-risk, CNN reported. For low-risk patients, the potential risks and benefits of surgery and radiation should be carefully weighed, since "more aggressive therapy can result in more harm than good," the study authors concluded.
No comments:
Post a Comment