BYCAROLYN BARBER
February 15, 2023

Wake Forest scientists are 3D-printing tissues and mini-organs that mimic some of the functional properties of our own natural tissues.
COURTESY OF WFIRM
Last year, in San Antonio, Texas, Dr. Arturo Bonilla carefully implanted an outer ear on a 20-year-old woman born without one. The ear on the woman’s right side, had been constructed in the size and shape of her left.
For Bonilla, a pediatric microtia surgeon (a doctor who treats birth defects of the ear) for more than 25 years and a recognized expert in the field, such a procedure would normally be routine. But this case had a twist: For the first time, the ear he was implanting was the product of a 3D bioprinter using the woman’s own cartilage cells.
The implant procedure, Bonilla told me, was “very uneventful.” It is a vast understatement, all things considered.
From the realm of near-fiction to the germ of an idea to actual science, 3D bioprinting is advancing across all aspects of medical research—and, now, practice. The pace is slow, and target dates for some of the most ambitious 3D plans are decades off. But progress is real.
“I think that in 10 years we will have organs for transplantation,” says professor Tal Dvir, director of tissue engineering and regenerative medicine at Tel Aviv University in Israel. “We will start with simple organs like skin and cartilage, but then we’ll move on to more complicated tissues—eventually the heart, liver, kidney.”
The future of 3D bioprinting
It sounds fantastical, but it’s already happening. Multilayered skin, bones, muscle structures, blood vessels, retinal tissue and even mini-organs all have been 3D printed. While none of the printed products are yet approved for human use, the race up the scientific timeline is breathtaking—and Bonilla’s ear procedure, the first 3D bioprint from live cells to be implanted in a human, marks a significant moment along that progression.
Researchers in Poland bioprinted a functional prototype of a pancreas in which stable blood flow was achieved in pigs during an observed two-week period, according to a 2022 abstract and Dr. Michal Wszola, creator of Bionic Pancreas. United Therapeutics Corporation has 3D printed a human lung scaffold with 4,000 kilometers of capillaries and 200 million alveoli (tiny air sacs) that are capable of oxygen exchange in animal models—a critical step toward creating tolerable, transplantable human lungs with the goal of being cleared for human trials within five years.
At Wake Forest Institute for Regenerative Medicine, scientists have developed a mobile skin bioprinting system. In the not-too-distant future, they anticipate being able to roll the printer right to the bedside of a patient suffering from a non-healing wound, such as a burn, then scan and measure the wound area and 3D print skin, layer by layer, directly onto the wound surface. And they’ve gone deeper, 3D printing skeletal muscle constructs that have been shown to contract in rodents and regain more than 80% of previously lost muscular function in an anterior leg muscle within eight weeks.
Dvir’s own lab has produced a 3D-printed “rabbit-sized” heart, as he puts it, replete with cells, chambers, the major blood vessels and a heartbeat. Full scale human hearts, the professor notes, require the same basic technology, although the process of scaling up is vastly complicated. “We’re now working on the pacemaker cells, the atrial cells, the ventricular cells,” Dvir says. “But it looks good. I believe this is the future.”
How 3D bioprinting works

Multilayered skin, bones, muscle structures, blood vessels, retinal tissue and even mini-organs all have been 3D printed. None are approved for human use yet.
COURTESY OF WFIRM
The ability to 3D print human organs is an astounding notion. Nearly 106,000 Americans are currently on waiting lists for organ donations, and 17 die each day while waiting, according to the federal Health Resources and Services Administration. A 3D printing process that uses the patient’s own cells to grow organs would not only potentially curb that waiting list, but dramatically reduce the chances of organ rejection and likely eliminate the need for harmful life-long immunosuppressive medication.
“The ability to place different cell types in precise locations to build up a complex tissue, and the capability of integrating blood vessels that can deliver the necessary oxygen and nutrients to keep cells alive, are two (3D) techniques that are revolutionizing tissue engineering,” says Mark Skylar-Scott, an assistant professor in the Stanford University department of bioengineering. “The field has moved very quickly over the past two decades, from printed bladders to now highly cellular tissues with vessels that can be connected to a pump—and complex 3D models that resemble heart components with integrated heart cells.”
In 3D bioprinting, the name of the game is cells. The process begins by generating the cells that researchers want to bioprint, which are then instructed to become organ specific cell types. The cells are then rendered into a printable living ink, or bioink, that involves mixing them with materials like gelatin or alginate to give them a toothpaste-like consistency. Stanford’s lab is studying how stem cells might naturally form such a consistency if crammed together at high density, which could lead to 3D printed organs made strictly from a patient’s own cells.
The bioink is loaded into syringes and squeezed out of a nozzle “like icing on a cake,” Skylar-Scott says. This is the actual 3D bioprinting process, and it typically involves laying down different cell types, each loaded into a different nozzle. (Dvir says the mini-heart took about four hours to print.) Once it is finished, the tissue is sometimes connected to a pump that drives oxygen and nutrients through it. Given time, the tissue develops on its own and increases in both maturity and function.
That general process, though dramatically oversimplified here, is what led to the production of the external part of the ear that Arturo Bonilla implanted in his patient in Texas. In most previous microtia surgeries, Bonilla would have carved a new ear out of cartilage taken from the patient’s ribs. Instead, a small biopsy was performed on the patient’s other ear and cartilage cells taken from the biopsy were grown into billions of cells, which were 3D-printed into the new implant.
“As with any study, there will likely be iterations in future patients in order to try to improve this technique,” Bonilla says. “We are unsure when this will be the mainstay treatment, but the future is very exciting.”
COURTESY OF WFIRM
The ability to 3D print human organs is an astounding notion. Nearly 106,000 Americans are currently on waiting lists for organ donations, and 17 die each day while waiting, according to the federal Health Resources and Services Administration. A 3D printing process that uses the patient’s own cells to grow organs would not only potentially curb that waiting list, but dramatically reduce the chances of organ rejection and likely eliminate the need for harmful life-long immunosuppressive medication.
“The ability to place different cell types in precise locations to build up a complex tissue, and the capability of integrating blood vessels that can deliver the necessary oxygen and nutrients to keep cells alive, are two (3D) techniques that are revolutionizing tissue engineering,” says Mark Skylar-Scott, an assistant professor in the Stanford University department of bioengineering. “The field has moved very quickly over the past two decades, from printed bladders to now highly cellular tissues with vessels that can be connected to a pump—and complex 3D models that resemble heart components with integrated heart cells.”
In 3D bioprinting, the name of the game is cells. The process begins by generating the cells that researchers want to bioprint, which are then instructed to become organ specific cell types. The cells are then rendered into a printable living ink, or bioink, that involves mixing them with materials like gelatin or alginate to give them a toothpaste-like consistency. Stanford’s lab is studying how stem cells might naturally form such a consistency if crammed together at high density, which could lead to 3D printed organs made strictly from a patient’s own cells.
The bioink is loaded into syringes and squeezed out of a nozzle “like icing on a cake,” Skylar-Scott says. This is the actual 3D bioprinting process, and it typically involves laying down different cell types, each loaded into a different nozzle. (Dvir says the mini-heart took about four hours to print.) Once it is finished, the tissue is sometimes connected to a pump that drives oxygen and nutrients through it. Given time, the tissue develops on its own and increases in both maturity and function.
That general process, though dramatically oversimplified here, is what led to the production of the external part of the ear that Arturo Bonilla implanted in his patient in Texas. In most previous microtia surgeries, Bonilla would have carved a new ear out of cartilage taken from the patient’s ribs. Instead, a small biopsy was performed on the patient’s other ear and cartilage cells taken from the biopsy were grown into billions of cells, which were 3D-printed into the new implant.
“As with any study, there will likely be iterations in future patients in order to try to improve this technique,” Bonilla says. “We are unsure when this will be the mainstay treatment, but the future is very exciting.”
Advantages of 3D printing

3D bioprinting enables scientists to more precisely engineer tissues.
COURTESY OF WFIRM
Wake Forest scientists have been lab growing organs and tissues for years. They’ve used 3D printing to create in the laboratory essentially a mini-kidney and a mini-liver. The next challenge: larger, solid structures that more fully mimic organ function. “We are far from achieving this goal at organ scale,” says Jennifer Lewis, Wyss Professor of Biologically Inspired Engineering, at Harvard University.
“We’ve been able to print flat structures like skin, tubular structures like blood vessels or hollow, non-tubular organs like a bladder,” says Anthony Atala, founding director of the Wake Forest Institute. The larger solid organs are different, Atala says, “because of the challenge with the vascularity or the nutrition. There’s so many cells per centimeter.”
In some ways with cell production, it’s a matter of quality. Scientists have been able to create a heart cell from stem cells, but not one that beats as strongly as your heart cells do. The same is true for liver cells (metabolism) and kidney cells (filtrate uptake). “In some ways,” Skyler-Scott says, “the 3D bioprinting field is waiting on the basic biologists to make their major breakthroughs.”
There’s also the issue of quantity. The creation of a heart would require “billions of cells – and you need different cells, even different cardiac cells,” says Tal Dvir. To make enough cells for a single organ, a facility would need a 10-liter stirred vat that might cost $5,000 per day to feed, for months on end according to Skyler-Scott. And the ultimate goal is thousands of organs a month, not one.
Beyond all that, there are the questions of how the tissue integrates into the body and how it is supported by the body, including complex networks of blood vessels, nerves and multiple cell types, says Dan Cohen, CEO and co-founder of 3D Bio Therapeutics. “It’s not to say it can’t be done,” says Cohen, who began working in the field of bioprinting 20 years ago, when it didn’t have a formal name. “I have a lot of hope for bioprinting and regenerative medicine more broadly.”
Even in the short term, progress is well marked. Researchers at Harvard, Lewis says, generated cardiac cells from human pluripotent stem cells, then seeded them on a bioengineered chip with integrated sensors that can track the beating tissue. This 3D-printed-heart-on-a-chip can be used to test various cardiac drugs for potentially toxic side effects and may alleviate the need for animal testing.(A similar ALS-on-a-chip technology is being used to screen for drug candidates and to better understand the underlying mechanisms of that disease.)
“The 3D printer gives you several advantages,” says Wake Forest’s Atala. “The first is scale-up, because instead of making these (tissues and organs) by hand one at a time, you can automate the printer to do it. The second thing is precision. We can more precisely locate the cells where they’re needed.”
There’s also the notion of lower overall cost, as 3D printing allows for that increased scale. There is what Atala calls “reproducibility,” a method of producing the same structure again and again. And in terms of organ transplant, a new organ made of a patient’s own cells makes rejection far less likely.
Most researchers put the idea of full-sized 3D-printed organ transplantation in humans at somewhere between 20 and 30 years away. “Eventually, looking ahead, we’ll not need donor hearts. We’ll not need livers,” Dvir says. “This is my opinion, and I’m optimistic, but I think that in less than 20 years we will have printed organs inside us.” That is science at work, not science fiction.
COURTESY OF WFIRM
Wake Forest scientists have been lab growing organs and tissues for years. They’ve used 3D printing to create in the laboratory essentially a mini-kidney and a mini-liver. The next challenge: larger, solid structures that more fully mimic organ function. “We are far from achieving this goal at organ scale,” says Jennifer Lewis, Wyss Professor of Biologically Inspired Engineering, at Harvard University.
“We’ve been able to print flat structures like skin, tubular structures like blood vessels or hollow, non-tubular organs like a bladder,” says Anthony Atala, founding director of the Wake Forest Institute. The larger solid organs are different, Atala says, “because of the challenge with the vascularity or the nutrition. There’s so many cells per centimeter.”
In some ways with cell production, it’s a matter of quality. Scientists have been able to create a heart cell from stem cells, but not one that beats as strongly as your heart cells do. The same is true for liver cells (metabolism) and kidney cells (filtrate uptake). “In some ways,” Skyler-Scott says, “the 3D bioprinting field is waiting on the basic biologists to make their major breakthroughs.”
There’s also the issue of quantity. The creation of a heart would require “billions of cells – and you need different cells, even different cardiac cells,” says Tal Dvir. To make enough cells for a single organ, a facility would need a 10-liter stirred vat that might cost $5,000 per day to feed, for months on end according to Skyler-Scott. And the ultimate goal is thousands of organs a month, not one.
Beyond all that, there are the questions of how the tissue integrates into the body and how it is supported by the body, including complex networks of blood vessels, nerves and multiple cell types, says Dan Cohen, CEO and co-founder of 3D Bio Therapeutics. “It’s not to say it can’t be done,” says Cohen, who began working in the field of bioprinting 20 years ago, when it didn’t have a formal name. “I have a lot of hope for bioprinting and regenerative medicine more broadly.”
Even in the short term, progress is well marked. Researchers at Harvard, Lewis says, generated cardiac cells from human pluripotent stem cells, then seeded them on a bioengineered chip with integrated sensors that can track the beating tissue. This 3D-printed-heart-on-a-chip can be used to test various cardiac drugs for potentially toxic side effects and may alleviate the need for animal testing.(A similar ALS-on-a-chip technology is being used to screen for drug candidates and to better understand the underlying mechanisms of that disease.)
“The 3D printer gives you several advantages,” says Wake Forest’s Atala. “The first is scale-up, because instead of making these (tissues and organs) by hand one at a time, you can automate the printer to do it. The second thing is precision. We can more precisely locate the cells where they’re needed.”
There’s also the notion of lower overall cost, as 3D printing allows for that increased scale. There is what Atala calls “reproducibility,” a method of producing the same structure again and again. And in terms of organ transplant, a new organ made of a patient’s own cells makes rejection far less likely.
Most researchers put the idea of full-sized 3D-printed organ transplantation in humans at somewhere between 20 and 30 years away. “Eventually, looking ahead, we’ll not need donor hearts. We’ll not need livers,” Dvir says. “This is my opinion, and I’m optimistic, but I think that in less than 20 years we will have printed organs inside us.” That is science at work, not science fiction.
General Atomics signs 3D printing agreement with automotive-focused startup Divergent
For something like a small UAS, “instead of taking years to develop [a design] it takes months, and instead of taking weeks to manufacture by laying out carbon fiber, we take hours to assemble," Divergent CEO Kevin Czinger told Breaking Defense.
By AARON MEHTA
“We believe digital manufacturing and 3-D printing technologies can provide a revolutionary leap forward in next-generation UAS development, and produce fast, impressive results at the lowest cost,” Brinkley said in a statement. “Integrating best-in-class technologies into our process is critical to that effort, and we hope to make some announcements on partnerships in the very near future.”
Teaming with Divergent could have obvious benefits for GA, both as a way to drive down costs on existing systems and as it keeps pace with the global demand for unmanned aerial vehicles — including the upcoming competition for the Air Force’s Collaborative Combat Aircraft program. The CCA effort, currently under development, is envisioned as a set of semi-autonomous, attritable drones designed to accompany next-generation fighter jets. The competition for those next-generation drones could begin in fiscal year 2024, Breaking Defense has reported.
In realistic terms, “attritable” means the system has to be cheap and easy to manufacture, because you expect to lose them during operations. While it’s unclear if CCA was a consideration in the partnership planning, if Czinger’s 3D printing can do what he claims, that would clearly fit the mold.
Another potential benefit, Czinger said, is his confidence that it would be easy to set up a Divergent printing system out in the field.
Recommended
The sights of IDEX 2023 Day 1 [PHOTOS]
Hundreds of companies from dozens of countries are showing off their latest tech and weapons systems in the United Arab Emirates.
It would take “weeks” to set up an assembly cell — a hexagonal structure about 22 meters wide — outside the US, which could then begin printing small UAV structures just about anywhere. While the payloads would still need to be assembled and loaded on by traditional methods, a field-production capability has long been the dream of 3D printing advocates. Czinger also pointed out that being downrange with such a setup means that military users could see how a UAV design was performing in the field, take that data in and quickly adjust the design as needed to counter enemy defensive systems.
Notably, Czinger said, he expects the defense and aerospace industry to become a “very significant market” for his company, which is part of the reason he recruited former chairman of the joint chiefs of staff Peter Pace to sit on the company’s board.
GA is “the first [defense] company we started working with, they’re the furthest along and we do have a development partnership with them,” he said, “but they’re not the only aerospace/defense company that we’re working with.”
For something like a small UAS, “instead of taking years to develop [a design] it takes months, and instead of taking weeks to manufacture by laying out carbon fiber, we take hours to assemble," Divergent CEO Kevin Czinger told Breaking Defense.
By AARON MEHTA
on February 15, 2023
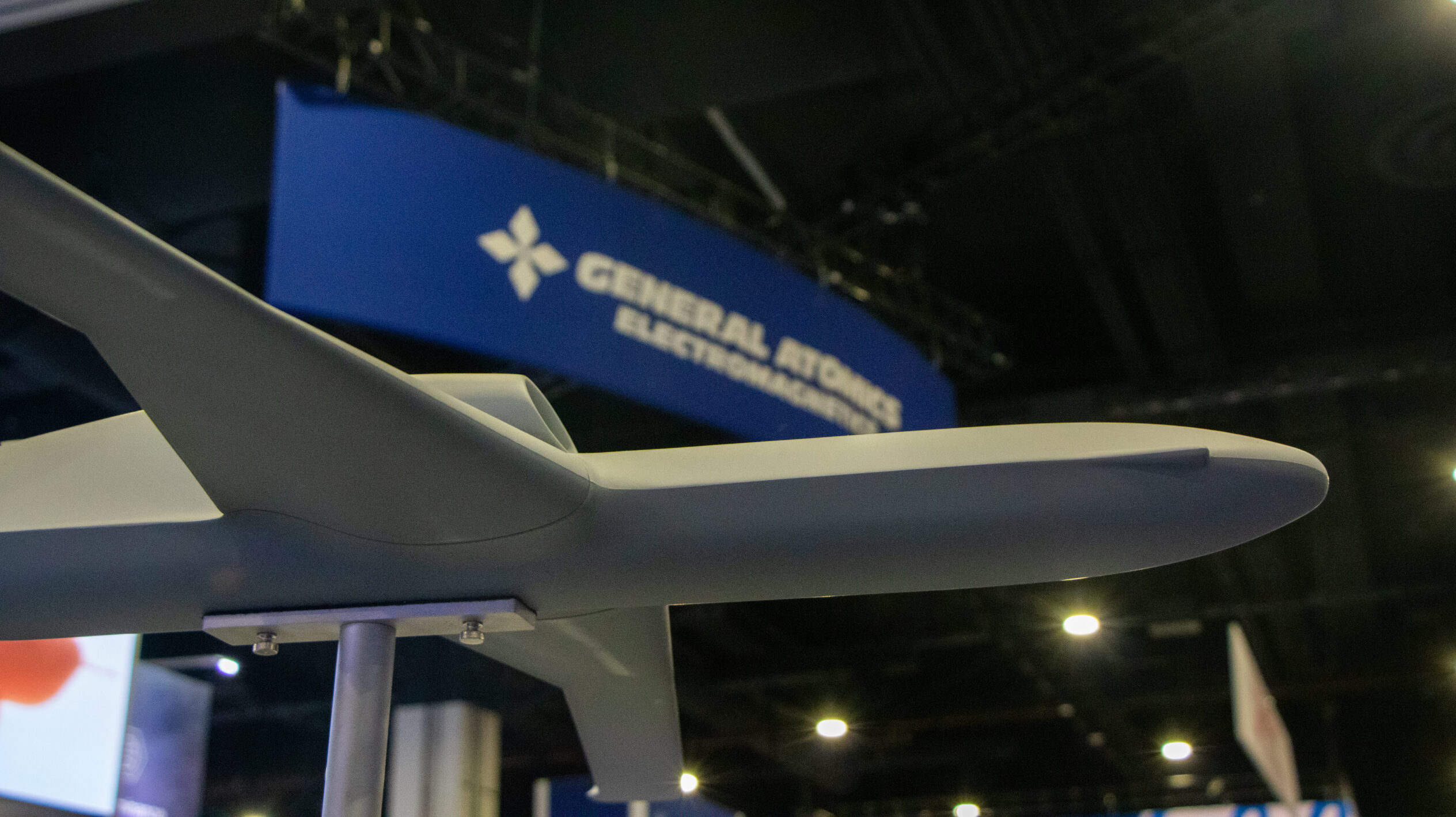
A General Atomics drone model at the AFA 2022 Air, Space and Cyber Conference. (Justin Katz/Breaking Defense)
WASHINGTON — Seeking cheaper, faster production for its unmanned vehicles, General Atomics plans to announce this week a new agreement with commercial automotive 3D printing firm Divergent Technologies, Breaking Defense has learned.
Divergent isn’t known in defense circles, but the company has made inroads in the commercial automotive industry. The startup has signed agreements with a number of car companies, and this year will have parts on the road in Aston Martin vehicles; it has gotten writeups in the New York Times and Forbes. Divergent founder Kevin Czinger has also launched his own line of 3D-printed supercars as a proof-of-concept. The company has raised roughly $700 million through series D funding.
Reached by phone today, Czinger confirmed the agreement with General Atomics. The goal, Czinger said, is for Divergent’s production process to take GA’s existing designs and use additive manufacturing to cut the process down dramatically in both time and cost.
“For example, their structure with fasteners is about 140 pieces for a small unmanned aerial system. We’re taking it down to four, by integrating different structures into the printed structure that we design, manufacture and assemble,” he said. “All of that is done in an automated way. “
For something like a small UAS, “instead of taking years to develop [a design], it takes months, and instead of taking weeks to manufacture by laying out carbon fiber, we take hours to assemble.”
While additive manufacturing is hardly a new technology, Czinger cites nearly 550 patented technologies as part of his technology stack, and claims the company’s production is “15-30 times faster than the fastest state of the art machine” available elsewhere.
Reached for comment, GA spokesman C. Mark Brinkley declined to discuss the Divergent agreement directly. But he did highlight the company’s September announcement of a new Additive Design and Manufacturing Center of Excellence as proof the company is a “disruptor” of traditional practices.
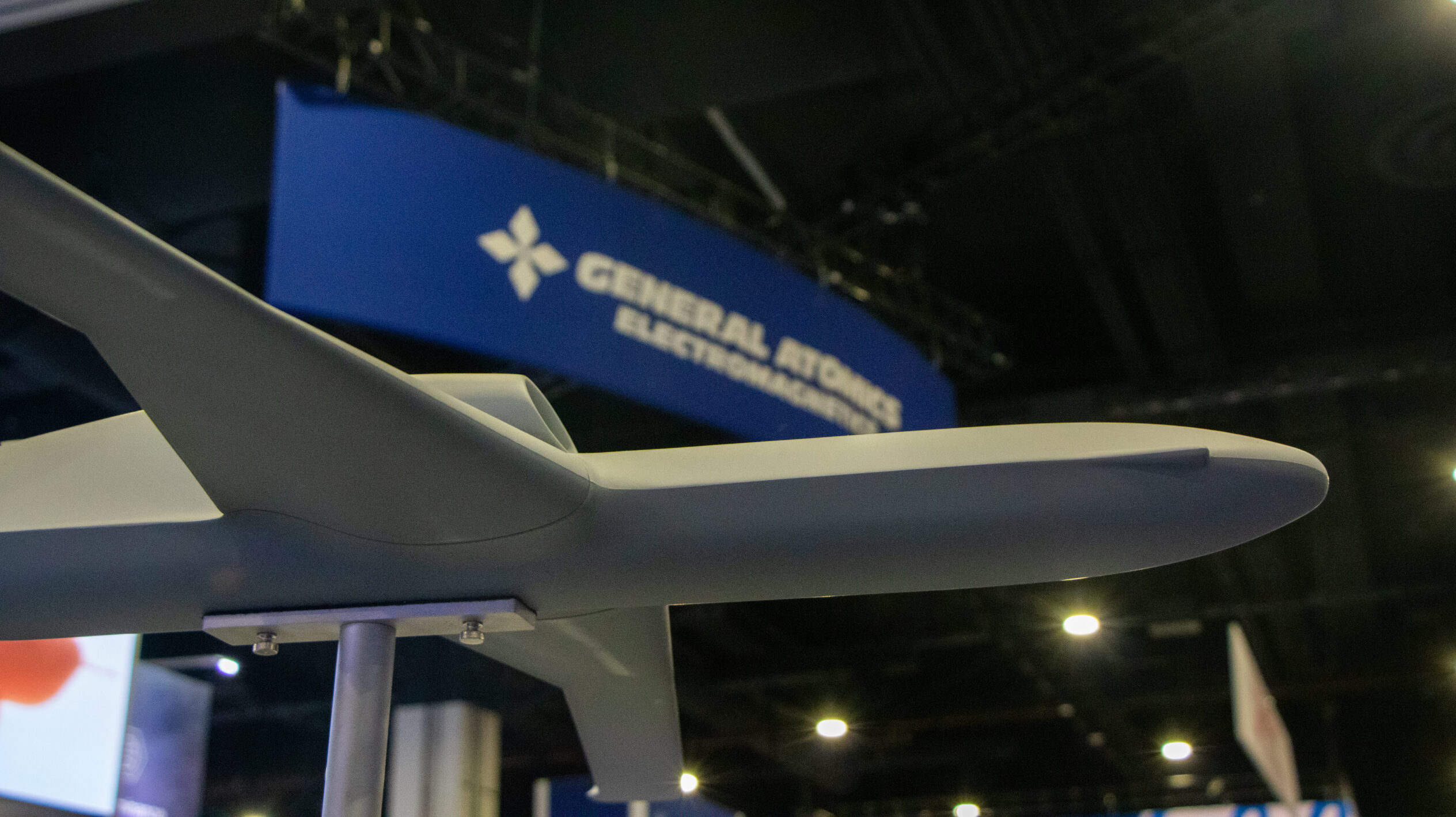
A General Atomics drone model at the AFA 2022 Air, Space and Cyber Conference. (Justin Katz/Breaking Defense)
WASHINGTON — Seeking cheaper, faster production for its unmanned vehicles, General Atomics plans to announce this week a new agreement with commercial automotive 3D printing firm Divergent Technologies, Breaking Defense has learned.
Divergent isn’t known in defense circles, but the company has made inroads in the commercial automotive industry. The startup has signed agreements with a number of car companies, and this year will have parts on the road in Aston Martin vehicles; it has gotten writeups in the New York Times and Forbes. Divergent founder Kevin Czinger has also launched his own line of 3D-printed supercars as a proof-of-concept. The company has raised roughly $700 million through series D funding.
Reached by phone today, Czinger confirmed the agreement with General Atomics. The goal, Czinger said, is for Divergent’s production process to take GA’s existing designs and use additive manufacturing to cut the process down dramatically in both time and cost.
“For example, their structure with fasteners is about 140 pieces for a small unmanned aerial system. We’re taking it down to four, by integrating different structures into the printed structure that we design, manufacture and assemble,” he said. “All of that is done in an automated way. “
For something like a small UAS, “instead of taking years to develop [a design], it takes months, and instead of taking weeks to manufacture by laying out carbon fiber, we take hours to assemble.”
While additive manufacturing is hardly a new technology, Czinger cites nearly 550 patented technologies as part of his technology stack, and claims the company’s production is “15-30 times faster than the fastest state of the art machine” available elsewhere.
Reached for comment, GA spokesman C. Mark Brinkley declined to discuss the Divergent agreement directly. But he did highlight the company’s September announcement of a new Additive Design and Manufacturing Center of Excellence as proof the company is a “disruptor” of traditional practices.
“We believe digital manufacturing and 3-D printing technologies can provide a revolutionary leap forward in next-generation UAS development, and produce fast, impressive results at the lowest cost,” Brinkley said in a statement. “Integrating best-in-class technologies into our process is critical to that effort, and we hope to make some announcements on partnerships in the very near future.”
Teaming with Divergent could have obvious benefits for GA, both as a way to drive down costs on existing systems and as it keeps pace with the global demand for unmanned aerial vehicles — including the upcoming competition for the Air Force’s Collaborative Combat Aircraft program. The CCA effort, currently under development, is envisioned as a set of semi-autonomous, attritable drones designed to accompany next-generation fighter jets. The competition for those next-generation drones could begin in fiscal year 2024, Breaking Defense has reported.
In realistic terms, “attritable” means the system has to be cheap and easy to manufacture, because you expect to lose them during operations. While it’s unclear if CCA was a consideration in the partnership planning, if Czinger’s 3D printing can do what he claims, that would clearly fit the mold.
Another potential benefit, Czinger said, is his confidence that it would be easy to set up a Divergent printing system out in the field.
Recommended
The sights of IDEX 2023 Day 1 [PHOTOS]
Hundreds of companies from dozens of countries are showing off their latest tech and weapons systems in the United Arab Emirates.
It would take “weeks” to set up an assembly cell — a hexagonal structure about 22 meters wide — outside the US, which could then begin printing small UAV structures just about anywhere. While the payloads would still need to be assembled and loaded on by traditional methods, a field-production capability has long been the dream of 3D printing advocates. Czinger also pointed out that being downrange with such a setup means that military users could see how a UAV design was performing in the field, take that data in and quickly adjust the design as needed to counter enemy defensive systems.
Notably, Czinger said, he expects the defense and aerospace industry to become a “very significant market” for his company, which is part of the reason he recruited former chairman of the joint chiefs of staff Peter Pace to sit on the company’s board.
GA is “the first [defense] company we started working with, they’re the furthest along and we do have a development partnership with them,” he said, “but they’re not the only aerospace/defense company that we’re working with.”



No comments:
Post a Comment