CDC reports the rich sleep better at night
by Bob Yirka , Medical Xpress

Credit: Pixabay/CC0 Public Domain
The U.S. Centers for Disease Control and Prevention has conducted a sleep study and found that rich people, on average, sleep longer at night than poor people. According to a report by CNN, researchers at the agency sent surveys to people in the United States over the years 2011 to 2014 inquiring about their sleep habits and have now made their results public.
The results showed that out of 140,000 adults who filled out and returned the surveys, 55% who reported living at or near the poverty line were able to get the recommended seven to eight hours of sleep at night. In contrast, for those living 400% above the poverty line, 66.6% reported getting a full night's sleep. The poverty line in the U.S. varies by income compared to family size. For a single person, it falls at $11,670 a year, while for a family of four, the number is $23,850.
Prior research has shown that chronic shortages of sleep can lead to many health problems, from high blood pressure to depression, obesity and diabetes. When combined with overall stress, it has been found to be a contributor to heart disease, cancer risk, a reduction in quality of life and a greater chance of dying.
Explore further
The U.S. Centers for Disease Control and Prevention has conducted a sleep study and found that rich people, on average, sleep longer at night than poor people. According to a report by CNN, researchers at the agency sent surveys to people in the United States over the years 2011 to 2014 inquiring about their sleep habits and have now made their results public.
The results showed that out of 140,000 adults who filled out and returned the surveys, 55% who reported living at or near the poverty line were able to get the recommended seven to eight hours of sleep at night. In contrast, for those living 400% above the poverty line, 66.6% reported getting a full night's sleep. The poverty line in the U.S. varies by income compared to family size. For a single person, it falls at $11,670 a year, while for a family of four, the number is $23,850.
The researchers did not dig deeper to discover why rich people sleep more, but some in the sleep field have suggested it is likely linked to the number of hours people have to work, or even the number of jobs. They also note that rich people have more help with childcare and other assistance with daily matters, such as cooking, cleaning and taking care of themselves. Rich people also tend to live in accommodations that are more receptive to sleep, such as quiet neighborhoods and private comfortable beds. The researchers also did not look into the impact of sleep differences between rich and poor on the country or the impact of chronic sleep deprivation on people living in sometimes desperate conditions. Also not mentioned was the impact the pandemic is having on the sleep patterns of people of both classes.
Prior research has shown that chronic shortages of sleep can lead to many health problems, from high blood pressure to depression, obesity and diabetes. When combined with overall stress, it has been found to be a contributor to heart disease, cancer risk, a reduction in quality of life and a greater chance of dying.
Explore further










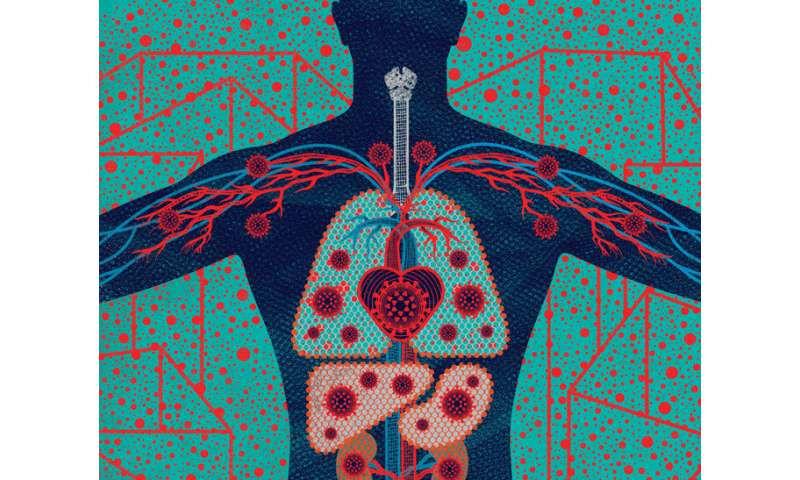

 From Head to “COVID Toes”: People with COVID-19 exhibit from none to many of these symptoms. Some symptoms (such as fever, cough, and loss of smell) are common, while others (such as sore throat, pink eye, and stroke) are rare. Credit: Illustration: Stephanie Koch. Concept: Jennifer Babik, M.D., Ph.D.
From Head to “COVID Toes”: People with COVID-19 exhibit from none to many of these symptoms. Some symptoms (such as fever, cough, and loss of smell) are common, while others (such as sore throat, pink eye, and stroke) are rare. Credit: Illustration: Stephanie Koch. Concept: Jennifer Babik, M.D., Ph.D.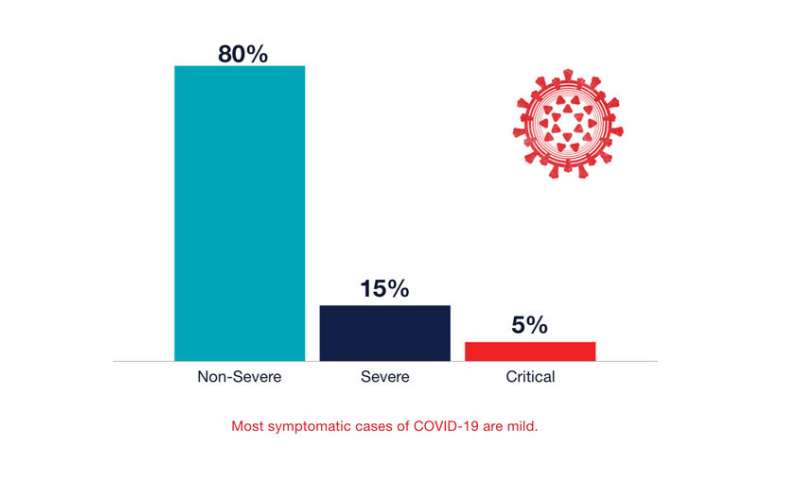 Most symptomatic cases of COVID-19 are mild. Credit: UCSF
Most symptomatic cases of COVID-19 are mild. Credit: UCSF