Three 103-year-old-lung samples hinted at how the flu mutated to become more deadly.
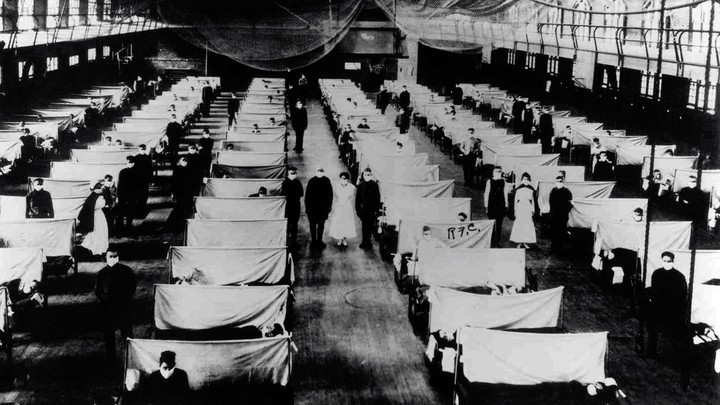
A converted warehouse that was used to isolate 1918 flu patients
UNIVERSAL HISTORY ARCHIVE / UNIVERSAL IMAGES GROUP / GETTY
The three teenagers—two boys and a girl—could not have known what clues their lungs would one day yield. All they could have known, or felt, before they died in Germany in 1918 was their flu-ravaged lungs failing them, each breath getting harder and harder. Tens of millions of people like them died in the flu pandemic of 1918; they happened to be three whose lungs were preserved by a farsighted pathologist.
A century later, scientists have now managed to sequence flu viruses from pea-size samples of the three preserved lungs. Together, these sequences suggest an answer to one of the pandemic’s most enduring mysteries: Why was the second wave, in late 1918, so much deadlier than the first wave, in the spring? These rediscovered lung samples hint at the possibility that the virus itself changed to better infect humans.
This might sound familiar. The no-longer-so-novel coronavirus is also adapting to its human host. With modern tools, scientists are tracking the virus’s evolution in real time and finding mutations that have made the virus better at infecting us. More than 1.4 million coronavirus genomes have now been sequenced. But the database for the 1918 flu is much smaller—so much so that the comparison feels unfair. This new study brings the number of complete 1918 flu genomes to a grand total of three, plus some partial genomes.
Hundred-year-old lung tissue is incredibly hard to find. Sébastien Calvignac-Spencer, a virologist at the Robert Koch Institute, in Berlin, came across the samples in this newest study in a stroke of luck. A couple of years ago, he decided to investigate the collections of the Berlin Museum of Medical History of the Charité. He wasn’t looking for anything in particular, but he soon stumbled upon several lung specimens from 1918, a year he of course recognized as a notable one for respiratory disease. Despite the flu pandemic’s notoriety, the virus that caused it is still poorly understood. “I thought, Well, okay, so it’s right here in front of you. Why don’t you give it a try?” he told me. Why not try to sequence influenza from these lungs? (This work is not dangerous: The chemically preserved lung specimens do not contain intact or infectious virus; sequencing picks up just fragments of the virus’s genetic material.)
Calvignac-Spencer and his colleagues ultimately tested 13 lung specimens and found evidence of flu in three. One was from a 17-year-old girl who died in Munich sometime in 1918. The two others were from teenage soldiers who both died in Berlin on June 27, 1918. This work is described in a new preprint, which has not yet been peer-reviewed.
The team was able to recover a complete flu-virus genome from the 17-year-old girl’s lung tissue—only the third ever found. The two other full 1918 flu genomes both came from the United States, from the lungs of a woman buried in Alaska and from a paraffin-wax-embedded lung sample of a soldier who died in New York. With another genome in hand, the researchers moved to investigate how they differed. Several changes showed up in the flu’s genome-replication machinery, a potential evolutionary hot spot because better replication means a more successful virus. The team then copied just the replication machinery of the 17-year-old’s virus—not the entire virus—into cells and found it was only half as active as that of the flu virus found in Alaska.
The obvious caveats should apply here: tiny sample size, the limits of extrapolating from test tube to human body. The exact date of the girl’s death in 1918 is also unknown, but this finding hints at the possibility that the virus’s behavior did change during the pandemic. Scientists have long speculated about why the 1918 pandemic’s second wave was deadlier than the first. Patterns of human behavior and seasonality could explain some of the difference—but the virus itself might have changed too. “And this starts to put some meat on the bone” of that hypothesis, Andrew Mehle, an influenza researcher at the University of Wisconsin at Madison, who was not involved in the study, told me.
The lungs of the two young soldiers in Berlin provide another clue. The teenagers’ June 1918 deaths were squarely in the pandemic’s first wave. These two samples yielded only partial genomes, but the team was able to reconstruct enough to home in on changes in nucleoprotein, one of the proteins that make up the virus’s replication machinery. Nucleoproteins act like scaffolds for the virus’s gene segments, which wind around the protein like a spiral staircase. They are also extremely distinctive, which can be a weakness: The human immune system is very good at recognizing and sabotaging them.
Indeed, the 1918 flu virus’s nucleoprotein seems to have mutated between the first and second waves to better evade the human immune system. The first-wave viruses’ nucleoproteins looked a bit like those in flu viruses that infect birds—which makes sense because scientists suspect that the 1918 flu originated in birds. But bird viruses are attuned to bird bodies. “When it jumps to humans, the virus is not evolved to be optimally resistant” to the human immune system, Jesse Bloom, a virologist at Fred Hutchinson Cancer Research Center, in Seattle, told me. Bloom and others have identified specific mutations that make the nucleoprotein better at resisting the human immune system. The first-wave flu viruses did not have them, but the second-wave ones did, possibly because they had had the time to adapt to infecting humans.
This mutation-by-mutation analysis of the 1918 flu virus would have been impossible to imagine at the time of the pandemic. Doctors then hadn’t even figured out that influenza was caused by a virus. “There’s no way the individual who saved these samples in 1918 had any idea of what could be done to them,” Mehle said. “To my mind, this is a beautiful example of fundamental research.” Without the pathologist who painstakingly preserved these samples and the museums that kept them for decades before science caught up, our understanding of the 1918 flu would be all the poorer.
Unfortunately, many historical samples have been lost as pathology collections have fallen out of fashion over the past century. “If we had started these kinds of studies in the ’60s, we would have had no problems finding thousands and thousands of specimens,” Calvignac-Spencer said. “And now we’re really fighting to assemble a collection of 20.” He’s been in touch with more than 50 museum collections around the world in the hunt for more pandemic-flu samples. He recently found one from Australia, but the work is slow. Calvignac-Spencer has also looked for other viruses, including measles, which he and his colleagues previously found in a 100-year-old lung from the same medical collection in Berlin.
The further back in time researchers must go, the harder the samples are to find—but Bloom told me he’s especially intrigued by the possibility of finding pre-1918 flu genomes in the archives. When the 1918 pandemic swept through the world, it apparently completely replaced whatever flu existed before. Its modern-day descendants continue to infect us today as seasonal flu. In this way, the 1918 flu is familiar to us and our immune systems. What came before is still a mystery.
The three teenagers—two boys and a girl—could not have known what clues their lungs would one day yield. All they could have known, or felt, before they died in Germany in 1918 was their flu-ravaged lungs failing them, each breath getting harder and harder. Tens of millions of people like them died in the flu pandemic of 1918; they happened to be three whose lungs were preserved by a farsighted pathologist.
A century later, scientists have now managed to sequence flu viruses from pea-size samples of the three preserved lungs. Together, these sequences suggest an answer to one of the pandemic’s most enduring mysteries: Why was the second wave, in late 1918, so much deadlier than the first wave, in the spring? These rediscovered lung samples hint at the possibility that the virus itself changed to better infect humans.
This might sound familiar. The no-longer-so-novel coronavirus is also adapting to its human host. With modern tools, scientists are tracking the virus’s evolution in real time and finding mutations that have made the virus better at infecting us. More than 1.4 million coronavirus genomes have now been sequenced. But the database for the 1918 flu is much smaller—so much so that the comparison feels unfair. This new study brings the number of complete 1918 flu genomes to a grand total of three, plus some partial genomes.
Hundred-year-old lung tissue is incredibly hard to find. Sébastien Calvignac-Spencer, a virologist at the Robert Koch Institute, in Berlin, came across the samples in this newest study in a stroke of luck. A couple of years ago, he decided to investigate the collections of the Berlin Museum of Medical History of the Charité. He wasn’t looking for anything in particular, but he soon stumbled upon several lung specimens from 1918, a year he of course recognized as a notable one for respiratory disease. Despite the flu pandemic’s notoriety, the virus that caused it is still poorly understood. “I thought, Well, okay, so it’s right here in front of you. Why don’t you give it a try?” he told me. Why not try to sequence influenza from these lungs? (This work is not dangerous: The chemically preserved lung specimens do not contain intact or infectious virus; sequencing picks up just fragments of the virus’s genetic material.)
Calvignac-Spencer and his colleagues ultimately tested 13 lung specimens and found evidence of flu in three. One was from a 17-year-old girl who died in Munich sometime in 1918. The two others were from teenage soldiers who both died in Berlin on June 27, 1918. This work is described in a new preprint, which has not yet been peer-reviewed.
The team was able to recover a complete flu-virus genome from the 17-year-old girl’s lung tissue—only the third ever found. The two other full 1918 flu genomes both came from the United States, from the lungs of a woman buried in Alaska and from a paraffin-wax-embedded lung sample of a soldier who died in New York. With another genome in hand, the researchers moved to investigate how they differed. Several changes showed up in the flu’s genome-replication machinery, a potential evolutionary hot spot because better replication means a more successful virus. The team then copied just the replication machinery of the 17-year-old’s virus—not the entire virus—into cells and found it was only half as active as that of the flu virus found in Alaska.
The obvious caveats should apply here: tiny sample size, the limits of extrapolating from test tube to human body. The exact date of the girl’s death in 1918 is also unknown, but this finding hints at the possibility that the virus’s behavior did change during the pandemic. Scientists have long speculated about why the 1918 pandemic’s second wave was deadlier than the first. Patterns of human behavior and seasonality could explain some of the difference—but the virus itself might have changed too. “And this starts to put some meat on the bone” of that hypothesis, Andrew Mehle, an influenza researcher at the University of Wisconsin at Madison, who was not involved in the study, told me.
The lungs of the two young soldiers in Berlin provide another clue. The teenagers’ June 1918 deaths were squarely in the pandemic’s first wave. These two samples yielded only partial genomes, but the team was able to reconstruct enough to home in on changes in nucleoprotein, one of the proteins that make up the virus’s replication machinery. Nucleoproteins act like scaffolds for the virus’s gene segments, which wind around the protein like a spiral staircase. They are also extremely distinctive, which can be a weakness: The human immune system is very good at recognizing and sabotaging them.
Indeed, the 1918 flu virus’s nucleoprotein seems to have mutated between the first and second waves to better evade the human immune system. The first-wave viruses’ nucleoproteins looked a bit like those in flu viruses that infect birds—which makes sense because scientists suspect that the 1918 flu originated in birds. But bird viruses are attuned to bird bodies. “When it jumps to humans, the virus is not evolved to be optimally resistant” to the human immune system, Jesse Bloom, a virologist at Fred Hutchinson Cancer Research Center, in Seattle, told me. Bloom and others have identified specific mutations that make the nucleoprotein better at resisting the human immune system. The first-wave flu viruses did not have them, but the second-wave ones did, possibly because they had had the time to adapt to infecting humans.
This mutation-by-mutation analysis of the 1918 flu virus would have been impossible to imagine at the time of the pandemic. Doctors then hadn’t even figured out that influenza was caused by a virus. “There’s no way the individual who saved these samples in 1918 had any idea of what could be done to them,” Mehle said. “To my mind, this is a beautiful example of fundamental research.” Without the pathologist who painstakingly preserved these samples and the museums that kept them for decades before science caught up, our understanding of the 1918 flu would be all the poorer.
Unfortunately, many historical samples have been lost as pathology collections have fallen out of fashion over the past century. “If we had started these kinds of studies in the ’60s, we would have had no problems finding thousands and thousands of specimens,” Calvignac-Spencer said. “And now we’re really fighting to assemble a collection of 20.” He’s been in touch with more than 50 museum collections around the world in the hunt for more pandemic-flu samples. He recently found one from Australia, but the work is slow. Calvignac-Spencer has also looked for other viruses, including measles, which he and his colleagues previously found in a 100-year-old lung from the same medical collection in Berlin.
The further back in time researchers must go, the harder the samples are to find—but Bloom told me he’s especially intrigued by the possibility of finding pre-1918 flu genomes in the archives. When the 1918 pandemic swept through the world, it apparently completely replaced whatever flu existed before. Its modern-day descendants continue to infect us today as seasonal flu. In this way, the 1918 flu is familiar to us and our immune systems. What came before is still a mystery.
No comments:
Post a Comment