Minorities at Greater Risk of Infection by Antimicrobial-Resistant Pathogens
Published on September 2, 2024
Reviewed By Gilmore Health |
Reviewed By Gilmore Health |
On: September 2, 2024
Table of Contents [show]
With the rise in the burden of contagious diseases, studies have shown that there exist some inequities in the colonization and infection of distinct races and ethnic groups by essential pathogens. Whether this is true for microbes that are becoming increasingly antimicrobial-resistant remains uncertain.
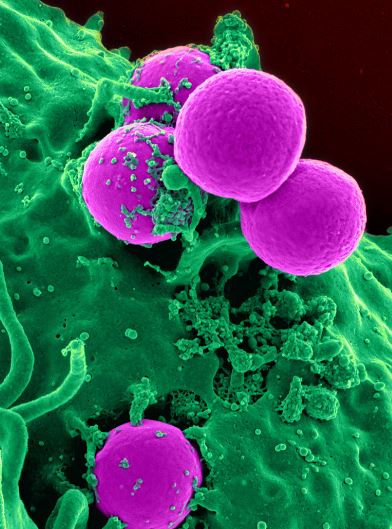
MRSA
Antimicrobial resistance develops when microbes no longer respond to antimicrobial therapy. These microbes are frequently community-acquired and gotten outside of healthcare environments. Many people who harbor these pathogens on their skin, gut, or mucosal surfaces tend to develop recurrent infections, stay longer in the hospital, and have a higher mortality rate.
This scoping study summarised the findings of several studies that assessed the relationship between race, ethnicity, and community-acquired infections and their disparities and identity gaps in their research.
Findings
The role of Social economic status (SES) and social determinants of health (SDOH)
Despite the establishment of the fact that differences/disparities exist in the way distinct ethnic and racial groups are colonized and infected by specific key pathogens, there has not been any clear biological rationale. However, these disparities have been linked to socioeconomic status characteristics such as low income, low educational achievement, lack of ease of access to health institutions, and overcrowding of residential areas. The cadre of people living in conditions such as these showed a higher risk of being colonized and developing an infection, even though there exists a social spectrum amongst individuals in the middle and upper classes of society.
The role of SES in health is rather contextual and depends on the environment in which a person lives. For example, an individual living in a country with a low income but easy accessibility to good healthcare facilities, good education, and other social services may be less at risk of being infected by these pathogens.
Race and ethnicity
This review included studies carried out in the USA, Australia, New Zealand, Brazil, and Israel. It noted that individuals belonging to the minority races/ethnic groups of these countries had a higher risk of being colonized or/and infected by these key pathogens, which are rapidly becoming AMR.
Gaps identified
In the studies examined, it was found that most did not consider the association between race, ethnicity, and SES but either examined race and ethnicity in conjunction or as independent variables from SES characters. This makes identifying a particular SES factor as the culprit for the disparities identified in this study difficult.
Only a minority of the studies considered, those conducted in New Zealand and Australia, included indigenous groups, making them poorly represented in this research.
It was found that first-nation populations in these countries had a higher risk of Staphylococcus aureus and methicillin-resistant S. aureus infections, supporting the necessity of research amongst the indigenous or minority races/ethnic groups in other countries.
Clinical significance
These findings help identify groups that would benefit from health policies tailored to improving their general health.
In communities where high-risk groups/races live, efforts should be made to educate individuals on proper hygiene and how to use antimicrobials to effectively limit the spread of antimicrobial-resistant pathogens.
This study has also revealed the necessity of upcoming research concerning race/ethnicity and infections to be more inclusive of the minority in order to collate better data that can be employed to provide better healthcare.
What Next?
With the establishment of the inequities in the colonization and infection of different race/ethnic groups, the role of SES towards general health outcomes, and the imbalance in the affectation of some minority groups, it is pertinent to embrace more inclusive criteria to research and overall healthcare provision.
References
Avendano, E. E., Blackmon, S. A., Nirmala, N., Chan, C. W., Morin, R. A., Balaji, S., McNulty, L., Argaw, S. A., Doron, S., & Nadimpalli, M. L. (2024). Race, ethnicity, and risk for colonization and infection with key bacterial pathogens: A scoping review.https://doi.org/10.1101/2024.04.24.24306289
Table of Contents [show]
With the rise in the burden of contagious diseases, studies have shown that there exist some inequities in the colonization and infection of distinct races and ethnic groups by essential pathogens. Whether this is true for microbes that are becoming increasingly antimicrobial-resistant remains uncertain.
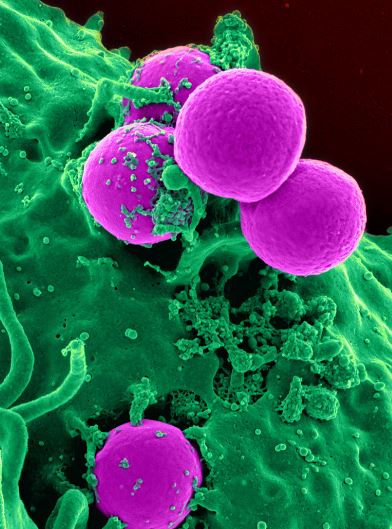
MRSA
Antimicrobial resistance develops when microbes no longer respond to antimicrobial therapy. These microbes are frequently community-acquired and gotten outside of healthcare environments. Many people who harbor these pathogens on their skin, gut, or mucosal surfaces tend to develop recurrent infections, stay longer in the hospital, and have a higher mortality rate.
This scoping study summarised the findings of several studies that assessed the relationship between race, ethnicity, and community-acquired infections and their disparities and identity gaps in their research.
Findings
The role of Social economic status (SES) and social determinants of health (SDOH)
Despite the establishment of the fact that differences/disparities exist in the way distinct ethnic and racial groups are colonized and infected by specific key pathogens, there has not been any clear biological rationale. However, these disparities have been linked to socioeconomic status characteristics such as low income, low educational achievement, lack of ease of access to health institutions, and overcrowding of residential areas. The cadre of people living in conditions such as these showed a higher risk of being colonized and developing an infection, even though there exists a social spectrum amongst individuals in the middle and upper classes of society.
The role of SES in health is rather contextual and depends on the environment in which a person lives. For example, an individual living in a country with a low income but easy accessibility to good healthcare facilities, good education, and other social services may be less at risk of being infected by these pathogens.
Race and ethnicity
This review included studies carried out in the USA, Australia, New Zealand, Brazil, and Israel. It noted that individuals belonging to the minority races/ethnic groups of these countries had a higher risk of being colonized or/and infected by these key pathogens, which are rapidly becoming AMR.
Gaps identified
In the studies examined, it was found that most did not consider the association between race, ethnicity, and SES but either examined race and ethnicity in conjunction or as independent variables from SES characters. This makes identifying a particular SES factor as the culprit for the disparities identified in this study difficult.
Only a minority of the studies considered, those conducted in New Zealand and Australia, included indigenous groups, making them poorly represented in this research.
It was found that first-nation populations in these countries had a higher risk of Staphylococcus aureus and methicillin-resistant S. aureus infections, supporting the necessity of research amongst the indigenous or minority races/ethnic groups in other countries.
Clinical significance
These findings help identify groups that would benefit from health policies tailored to improving their general health.
In communities where high-risk groups/races live, efforts should be made to educate individuals on proper hygiene and how to use antimicrobials to effectively limit the spread of antimicrobial-resistant pathogens.
This study has also revealed the necessity of upcoming research concerning race/ethnicity and infections to be more inclusive of the minority in order to collate better data that can be employed to provide better healthcare.
What Next?
With the establishment of the inequities in the colonization and infection of different race/ethnic groups, the role of SES towards general health outcomes, and the imbalance in the affectation of some minority groups, it is pertinent to embrace more inclusive criteria to research and overall healthcare provision.
References
Avendano, E. E., Blackmon, S. A., Nirmala, N., Chan, C. W., Morin, R. A., Balaji, S., McNulty, L., Argaw, S. A., Doron, S., & Nadimpalli, M. L. (2024). Race, ethnicity, and risk for colonization and infection with key bacterial pathogens: A scoping review.https://doi.org/10.1101/2024.04.24.24306289
No comments:
Post a Comment