1%PARASITE QUE JUMPERS
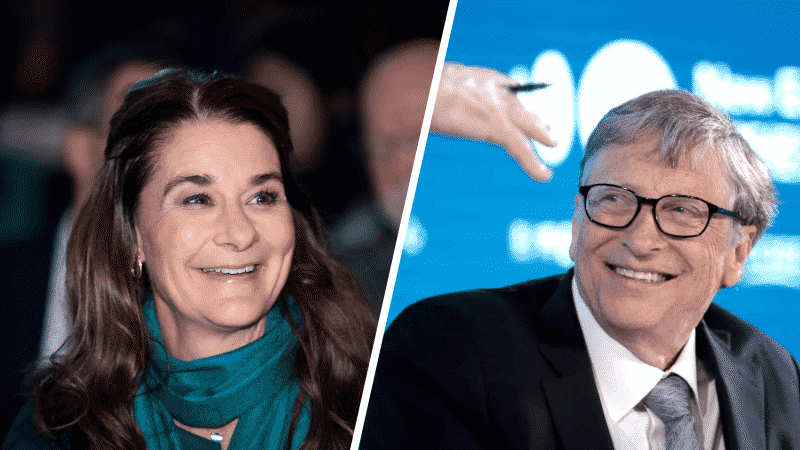
Bill and Melinda Gates Point To a New Injustice COVID Pandemic Could ‘Unleash’
Bill and Melinda Gates are expressing their concerns about a new injustice the COVID-19 pandemic could potentially lead to.
“Bill and I are deeply concerned, though, that in addition to shining a light on so many old injustices, the pandemic will unleash a new one: immunity inequality, a future where the wealthiest people have access to a COVID-19 vaccine, while the rest of the world doesn’t,” they warned in their annual letter on Wednesday.
They continued, “Until vaccines reach everyone, new clusters of disease will keep popping up. Those clusters will grow and spread. Schools and offices will shut down again. The cycle of inequality will continue.”
The couple argued the future depends on “whether the world comes together to ensure that the lifesaving science developed in 2020 saves as many lives as possible in 2021.”
Bill Gates said the world “failed to prepare” for the COVID-19 pandemic, but there is hope.
“To prevent the hardship of this last year from happening again, pandemic preparedness must be taken as seriously as we take the threat of war,” Bill Gates wrote.
He acknowledged the cost of the pandemic and suggested the world needs to spend “billions to save trillions (and prevent millions of deaths).”
Bill Gates advocated for creating a global alert system to spot outbreaks as soon as they happen.
He is optimistic the world will be better prepared to take on the next pandemic for one reason.
“The world now understands how seriously we should take pandemics. No one needs to be convinced that an infectious disease could kill millions of people or shut down the global economy,” Bill Gates wrote.
He added, “The pain of this past year will be seared into people’s thinking for a generation.”
They predicted the pandemic will serve as “a testament to the remarkable leaders” who put their lives at risk to help others.