Posted on June 12, 2020 by BJSM
Many community-based measures to control the spread of the coronavirus disease 19 (COVID-19) are implemented, including social distancing, hand hygiene and wearing non-medical face masks in public areas. This recommendation is based on the concept of ‘source control’ to prevent droplets produced by the person wearing the mask from spreading to other people or onto surfaces. It is much easier to reduce droplet spread by blocking larger droplets as they come out of a person’s mouth, that it is to block them as they have dissipated and become much smaller1.
Compulsory wearing of face masks is observed in some countries, e.g. South Africa, Taiwan, Japan, and the Czech Republic, and coincides with a reduction in rates of transmission1. However, adhering to these measures becomes more challenging and confusing during an outdoor exercise session. Infection control remains an important consideration, but wearing a mask comes with issues of potential breathing restriction and discomfort in mind. Selecting an appropriate face-covering becomes an act of balancing benefits versus possible adverse events. Most people will be able to exercise safely wearing a face covering, but points to consider include:
Viral transmission from infected but asymptomatic or pre-symptomatic individuals is possible.2,3,4 Due to the increased rate and force associated with breathing during exercise, the risk of aerolisation and the spread of virus-containing droplets could theoretically be higher than when at rest.
Reserve filtering facepiece respirators (FFRs) (e.g. N95/FFP1/FFP2) for specific work environments such as front-line healthcare workers. These should not be used by the public and also not for exercise purposes.
Airflow-restricting masks can increase the rate of perceived exertion and decrease performance during resistance training.5,6 Not much is known about the effect during aerobic activity. Surgical masks may increase perceptions of dyspnoea, but negative effects on aerobic performance have not been demonstrated.7
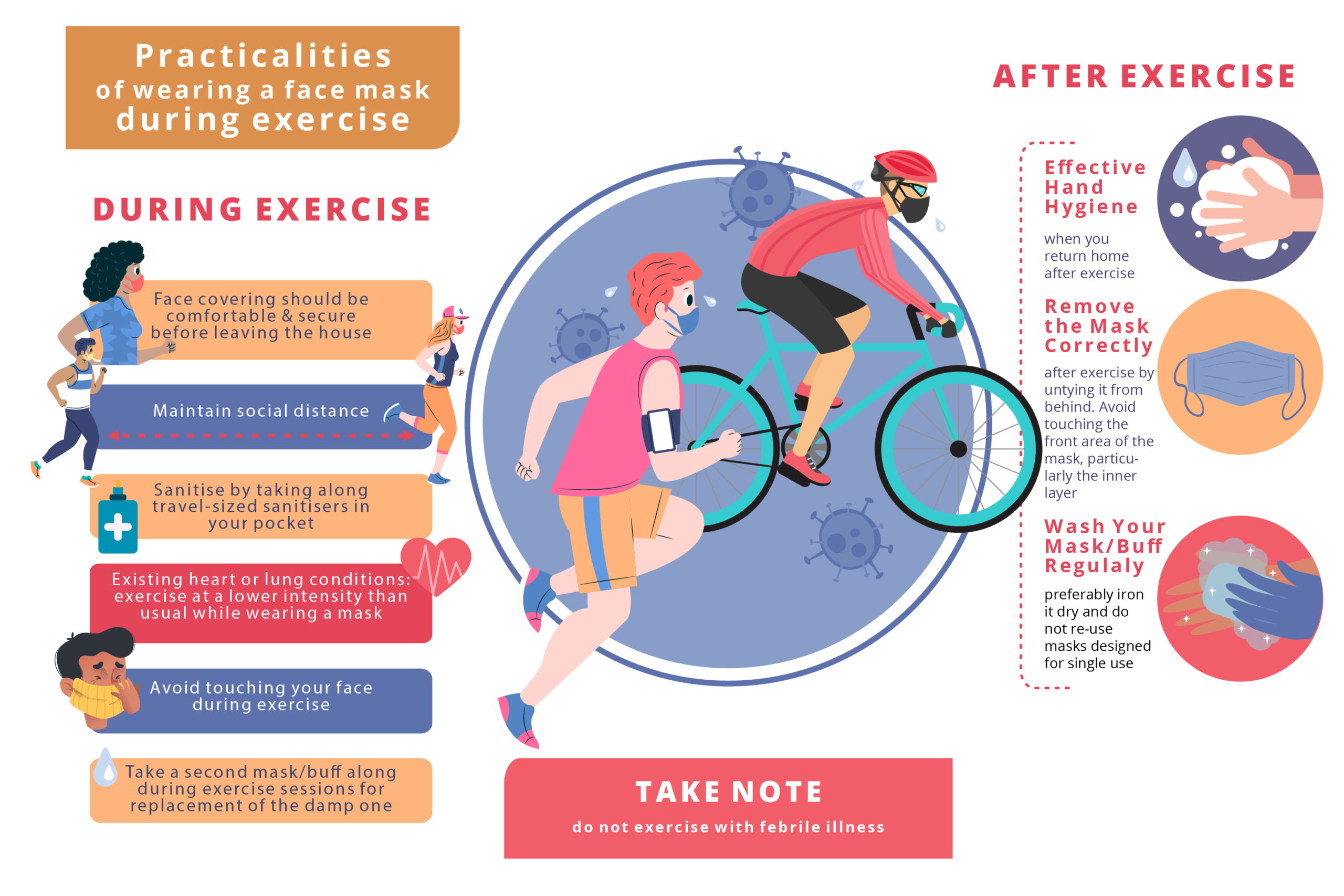
While there is no evidence showing the effects of cloth masks or buffs, they could potentially increase the breathing effort and cause accumulation of CO2. Wearing a mask may, in fact, simulate the physiological effect of altitude training, albeit on a smaller scale8. This is unlikely to be an issue for most people but could present a problem at higher intensities of exercise, particularly for those with underlying health concerns. It would be prudent for people with existing heart or lung conditions to exercise at a lower intensity than usual while wearing a mask, to prevent any adverse events. People must be cognisant of their breathing during exercise and somewhat slow down or take a break if they feel that their work rate is too high or if experiencing dizziness or light-headedness.
A more breathable material will aid in comfort but may have the cost of less effective viral source control. Two layers of material are considered sufficient to balance efficacy and comfort. Not having a tight seal around the sides of your face also allows for better air movement, but will subsequently increase the risk of droplet spread.
Due to the accumulation of moisture from our exhaled breath, cloth masks or buffs are likely to get wet during exercise. Breathing through dry cloth is easier as opposed to damp cloth. Hot and humid conditions can worsen the effect of strenuous breathing. Moisture-wicking material, such as polyester, is a good option but may cause skin irritation in sensitive individuals. Consider taking a second mask/buff along during exercise sessions for replacement of the damp one. This can be tricky as one should try to avoid touching your face. Therefore an attempt to maintain good hand hygiene before and after touching your face is advised and can be achieved by taking along travel-sized sanitisers in your pocket.
Theoretically, wet material may facilitate viral transmission. However, cloth masks are recommended for source control and are likely insufficient to prevent transmission of viral particles to the wearer even when dry.
Ensure that your face covering is comfortable and secure before leaving the house, to limit the need to readjust it and touch your face.
Although everything regarding COVID-19 is not clear yet, the rule not to exercise when suffering from febrile illness remains, due to the cardiorespiratory complications that may occur.9-10
Summary:
A face-covering is an effective way to prevent viral transmission in a community context, provided that compliance is high11.
This must be accompanied by social distancing during exercise and effective hand hygiene when you return home.
Remove the mask correctly after workouts by untying it from behind. Avoid touching the front area of the cover, particularly the inner layer.
After removing the mask, or in case of inadvertent touching it, wash or sanitise your hands.
Remember to wash your mask/buff regularly, preferably iron it dry, and do not re-use masks designed for single use.
Do not exercise with febrile illness.
Authors and Affiliations:
Jessica Hamuy Blancoa [MBBCh, DA (SA)]
Dina C (Christa) Janse van Rensburga, b [MD (PhD), MMed, MSc, MBChB, FACSM, FFIMS]
aSection Sports Medicine & Sport Exercise Medicine Lifestyle Institute (SEMLI), Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
bInternational Netball Federation, Manchester, UK Medical Board Member, UK
Email: christa.jansevanrensburg@up.ac.za
ORCID IDs
Jessica Hamuy Blanco – ORCID ID: 0000-0002-8035-1438
Dina C (Christa) Janse Van Rensburg – ORCID ID: 0000-0003-1058-6992
Twitter:
Jessica Hamuy Blanco – @JHamuyBlanco
Dina C (Christa) Janse Van Rensburg – @ChristaJVR
References:
Greenhalgh T. Face coverings for the public: Laying straw men to rest. J Eval Clin Pract. 2020.
Rothe C, et al. Transmission of 2019-ncov infection from an asymptomatic contact in germany. The New England journal of medicine. 2020; 382(10):970-1.
Pan X, et al. Asymptomatic cases in a family cluster with sars-cov-2 infection. The Lancet. Infectious diseases. 2020; 20(4):410-1.
Kimball A, et al. Asymptomatic and presymptomatic sars-cov-2 infections in residents of a long-term care skilled nursing facility. MMWR. Morbidity and mortality weekly report. 2020; 69(13):377-81.
Motoyama YL, et al. Airflow-restricting mask reduces acute performance in resistance exercise. Sports (Basel, Switzerland). 2016; 4(4):46.
Andre TL, et al. Restrictive breathing mask reduces repetitions to failure during a session of lower-body resistance exercise. J Strength Cond Res. 2018; 32(8):2103-8. Person E, et al. [effect of a surgical mask on six minute walking distance]. Rev Mal Respir. 2018; 35(3):264-8.
Burtscher M, et al. Effects of intermittent hypoxia on running economy. Int J Sports Med. 2010; 31(9).
Phelan D, et al. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (covid-19) infection. JAMA Cardiology. 2020.
Al-Qahtani AA. Severe acute respiratory syndrome coronavirus 2 (sars-cov-2): Emergence, history, basic and clinical aspects. Saudi J Biol Sci. 2020.
Howard J, et al. Face masks against covid-19: An evidence review. 2020.
No comments:
Post a Comment