Eyeing a cure: Scientists examine strategies to end the global HIV/AIDS pandemic
As infectious diseases that are new to science continue emerging around the world, researchers have not forgotten older foes, and are doubling down on efforts to conquer them. For HIV/AIDS, they've begun looking toward a cure.
Writing in the journal Nature, a team of three infectious disease experts from the United States and abroad assessed potential drug candidates in the pharmaceutical pipeline that might eradicate the virus. Their aim was deceptively simple—to underscore why and where a cure is needed and how it might be achieved.
A key take-home message from the authors, who hail from the University of California, San Francisco, the African Research Institute in Durban, South Africa, and the Bill and Melinda Gates Foundation in Seattle, was that much of the HIV cure research is underway in countries where HIV/AIDS doesn't dominate vital statistics.
"Cure research remains focused in academic medical centers located in low-HIV-burden, resource-rich countries," wrote Dr. Steven G. Deeks of UC San Francisco, who along with his two colleagues, contend that cutting-edge innovation must take into account the needs and economies of people who need it most.
"There has been limited public discussion on the practicalities of product development, particularly as they relate to sub-Saharan Africa," Deeks, and his colleagues Dr. Thumbi Ndung'u of the African Research Institute and Joseph M. McCune of the Gates Foundation noted. "Failure early on to define a target product-profile risks developing a strategy that fails to be effective."
The vast majority of global HIV/AIDS cases are concentrated in sub-Saharan Africa, according to the World Health Organization, where an estimated 65 percent of new infections and 75 percent of deaths caused by the virus occur. No other region of the world has greater need for a cure, experts say.
Hopes of snuffing out the viral cause of the global epidemic have emerged in earnest as scientists have begun testing variations on cancer immunotherapy and other groundbreaking approaches. Among evolving techniques under investigation is use of the gene-editing tool CRISPR-Cas9.
In October, scientists at the Gladstone Institutes in San Francisco reported in the journal Cell on a novel version of CAR-T cell therapy as a method of tackling HIV-infected cells.
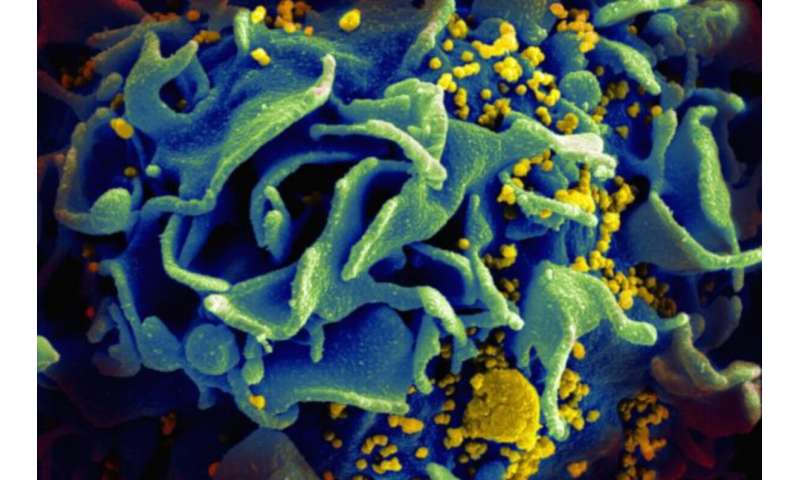
CAR-T therapy is used to treat cancers of the blood by supercharging a patient's own T cells in a lab. The T cells are re-infused into the patient as emboldened fighters capable of zeroing in on a specific cancer biomarker. With HIV, Gladstone researchers are supercharging immune cells and proteins to seek out latent HIV that's hiding in the body, eluding detection by the immune system.
The Gladstone research and emerging technologies are offering fresh approaches to an infectious disease that has claimed 32 million lives globally since 1981, according to WHO. In the United States alone, 700,000 people have lost their lives to HIV within the same time period, data from the Centers for Disease Control and Prevention show.
Although current antiretroviral therapy (ART) has allowed many patients to reduce viremia—the amount of virus in the blood—to undetectable levels, the medications are not cures, despite their effectiveness. Deeks and colleagues who analyzed HIV-treatment technologies in the journal Nature say emerging treatments aimed at curing HIV must be practical as well as effective.
ART therapies, for example, can number as few as a single pill per day. But while the treatment can decrease viral load to infinitesimal levels, the expense of daily lifelong medication necessitates the need for a cure, the three researchers contend.
Assessment of potential cures by Deeks and his co-authors included several possibilities that ranged from gene modification to cell therapy, among others. CRISPR-based approaches could be designed to target and excise the integrated provirus, and likely would be curative, the scientists predicted.
But the new technology is being pursued amid a staggering statistic: Despite tens of millions of HIV infections worldwide since the 1980s, only two people to date have been declared cured of the disease. Both are known by the cities where their cures occurred: The Berlin Patient and the London Patient.
Each underwent a bone marrow transplant, a treatment that is expensive, highly specialized and required meeting strict criteria. Bone marrow transplants are not a feasible method for addressing HIV, doctors say.
As it turned out, neither patient underwent bone marrow transplantation with the aim of being cured of HIV. Both were infused with donor bone marrow to treat cancer of the blood. Both disorders—their cancers and the HIV—went into remission. The HIV cures for both patients came as a surprise, doctors for the two patients have said.
The Berlin Patient was declared cured in 2007; the London Patient in 2019. The case study of the London patient was reported at the Conference on Retroviruses and Opportunistic Infections, which was held in Seattle last March.
As scientists move forward on a variety of cure-oriented research projects, it is important not to repeat past inequities should a cure emerge, according to the report in Nature.
"Only 60 percent of people who live with HIV [worldwide] currently receive antiretroviral therapy," Deeks and his colleagues wrote in the journal.
The remaining 40 percent, which amounts to millions of people, are intermittently treated or go without medication altogether. That vast swath of patients largely resides in the Southern Hemisphere.
No comments:
Post a Comment