Perfect storm: Lombardy's virus disaster is lesson for world
by Nicole Winfield APRIL 26, 2020

In this April 16, 2020 file photo, medical staff tend to a patient in the emergency COVID-19 ward at the San Carlo Hospital in Milan, Italy. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly clear that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. By contrast, Lombardy's front-line doctors and nurses are being hailed as heroes for risking their lives to treat the sick under extraordinary levels of stress, exhaustion, isolation and fear. (AP Photo/Antonio Calanni, file)
As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly clear that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country.
Italy had the bad luck of being the first Western nation to be slammed by the outbreak, and its official total of 26,000 fatalities lags behind only the U.S. in the global death toll. Italy's first homegrown case was recorded Feb. 21, at a time when the World Health Organization was still insisting the virus was "containable" and not nearly as infectious as the flu.
But there is also evidence that demographics and health care deficiencies collided with political and business interests to expose Lombardy's 10 million people to COVID-19 in ways unseen anywhere else, particularly the most vulnerable in nursing homes.
Virologists and epidemiologists say what went wrong there will be studied for years, given how the outbreak overwhelmed a medical system long considered one of Europe's best, while in neighboring Veneto, the impact was significantly more controlled.
Prosecutors, meanwhile, are deciding whether to lay any criminal blame for the hundreds of dead in nursing homes, many of whom don't even figure into Lombardy's official death toll of 13,269, half of Italy's total.
By contrast, Lombardy's front-line doctors and nurses are being hailed as heroes for risking their lives to treat the sick under extraordinary levels of stress, exhaustion, isolation and fear. One WHO official said it was a "miracle" they saved as many as they did.
Here's a look at the perfect storm of what went wrong in Lombardy, based on interviews and briefings with doctors, union representatives, mayors and virologists, as well as reports from Italy's Superior Institute of Health, national statistics agency ISTAT and the Organization for Economic Cooperation and Development, which advises developed economies on policy.

In this Feb. 28, 2020 file photo, a sunny day is reflected in a restaurant window where a sign with a hashtag reads "Milan doesn't stop" as a pizza maker puts a pizza in an oven, in Milan, Italy, As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. Unions and mayors of some of Lombardy's hardest hit cities say the country's main industrial lobby group, Confindustria, exerted enormous pressure on authorities to resist lockdowns and production shutdowns on the grounds that the economic cost would be too great in a region responsible for 21% of Italy's GDP. (AP Photo/Luca Bruno, file)
CAUGHT UNPREPARED
Italy was the first European country to halt all air traffic with China on Jan. 31, and even put scanners in airports to check arrivals for fever. But by Jan. 31, it was already too late. Epidemiologists now say the virus had been circulating widely in Lombardy since early January, if not before.
Doctors treating pneumonia in January and February didn't know it was the coronavirus, since the symptoms were so similar and the virus was still believed to be largely confined to China. Even after Italy registered its Feb. 21 case, doctors didn't understand the unusual way COVID-19 could present itself, with some patients experiencing a rapid decline in their ability to breathe.
"After a phase of stabilization, many deteriorated quickly. This was clinical information we didn't have," said Dr. Maurizio Marvisi, a pneumologist at a private clinic in hard-hit Cremona. "There was practically nothing in the medical literature."
Because Lombardy's intensive care units were already filling up within days of Italy's first cases, many primary care physicians tried to treat and monitor patients at home. Some put them on supplemental oxygen, commonly used for home cases in Italy.
That strategy proved deadly, and many died at home or soon after hospitalization, having waited too long to call an ambulance.
Reliance on home care "will probably be the determining factor of why we have such a high mortality rate in Italy," Marivi said.

In this Thursday, March 12, 2020 file photo, a worker wearing a mask and protective clothing walks between the emergency structures that were set up to ease procedures at the Brescia hospital in northern Italy. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly clear that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. (AP Photo/Luca Bruno)
Italy was forced to use home care in part because of its low ICU capacity: After years of budget cuts, Italy entered the crisis with 8.6 ICU beds per 100,000 people, well below the OECD average of 15.9 and a fraction of Germany's 33.9, the group said.
As a result, primary care physicians became the front-line filter of virus patients, an army of mostly self-employed practitioners who work within the public health system but outside Italy's regional hospital network.
Since only those with strong symptoms were being tested because Lombardy's labs couldn't process more, these family doctors didn't know if they themselves were infected, much less their patients.
With so little clinical information available, doctors also had no guidelines on when to admit patients or refer them to specialists. And being outside the hospital system, they didn't have the same access to protective masks and equipment.
"The region was extremely behind in giving us protective equipment and it was inadequate, because the first time, they gave us 10 surgical masks and gloves," said Dr. Laura Turetta in the city of Varese. "Obviously for our close contact with patients, it wasn't the correct way to protect ourselves."
The Lombardy doctors' association issued a blistering letter April 7 to regional authorities listing seven "errors" in their handling of the crisis, key among them the lack of testing for medical personnel, the lack of protective equipment and the lack of data about the contagion.
The regional government and civil protection agency defended their efforts, but acknowledged that Italy was dependent on imports and donations of protective equipment and simply didn't have enough to go around.

In this Feb. 28, 2020 file photo, people enjoy a sunny day while sitting at a cafe, in Milan, Italy. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. Unions and mayors of some of Lombardy's hardest hit cities say the country's main industrial lobby group, Confindustria, exerted enormous pressure on authorities to resist lockdowns and production shutdowns on the grounds that the economic cost would be too great in a region responsible for 21% of Italy's GDP. (AP Photo/Luca Bruno, file)Some 20,000 Italian medical personnel have been infected and 150 doctors have died.
LOST WEEKS
Two days after registering Italy's first case in the Lombardy province of Lodi, sparking a quarantine in 10 towns, another positive case was registered more than an hour's drive away in Alzano in Bergamo province. Whereas the emergency room of the Lodi-area hospital was closed, the Alzano ER reopened after a few hours of cleaning, becoming a main source of contagion.
Internal documents cited by Italian newspapers indicate the handful of serious pneumonia cases the Alzano hospital saw as early as Feb. 12 were likely COVID-19. At the time, Italy's health ministry recommended tests only for people who had been to China or been in contact with a suspected or confirmed positive case.
By March 2, the Superior Institute of Health recommended Alzano and nearby Nembro be sealed off as the towns in Lodi had been. But political authorities never implemented the quarantine recommendation there, allowing the infection to spread for a second week until all the Lombardy region was locked down March 7.
"The army was there, prepared to do a total closure, and if it had been done immediately maybe they could have stopped the contagion in the rest of Lombardy," said Dr. Guido Marinoni, head of the association of doctors in Bergamo province. "This wasn't done, and they took softer measures in all of Lombardy, and this allowed for the spread."
Asked why he didn't seal off Bergamo sooner, Premier Giuseppe Conte argued the regional government could have done so on its own. Lombardy's governor, Attilio Fontana, shot back that any mistake "was made by both. I don't think that there was blame in this situation.''

In this April 14, 2020 file photo, a car gets out of the Pio Albergo Trivulzio eldercare facility, in Milan, Italy. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly gistered more dead in nursing homes than any other region, nearly half of the 6,773 dead registered from Feb. 1-April 15, 40% of whom were either positive or had COVID-19 symwrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. Lombardy reptoms, according to a survey of the Superior Institutes of Health. (AP Photo/Luca Bruno, file)
Lombardy has one-sixth of Italy's 60 million people and is the most densely populated region, home to the business capital in Milan and the country's industrial heartland. Lombardy also has more people over 65 than any other Italian region, as well as 20% of Italy's nursing homes, a demographic time bomb for COVID-19 infections.
"Clearly, with the benefit of hindsight, we should have done a total shutdown in Lombardy, everyone at home and no one moves," said Andrea Crisanti, a microbiologist and virologist advising the Veneto regional government. But he acknowledged how hard that was, given Lombardy's outsize role in the Italian economy, which even before the pandemic was heading toward a recession.
"Probably for political reasons, it wasn't done," he told reporters.
INDUSTRIAL LOBBYING
Unions and mayors of some of Lombardy's hardest hit cities now say the country's main industrial lobby group, Confindustria, exerted enormous pressure to resist lockdowns and production shutdowns because the economic cost would be too great in a region responsible for 21% of Italy's GDP.
On Feb. 28, a week into the outbreak and well after more than 100 cases were registered in Bergamo, the province's branch of Confindustria launched an English-language social media campaign, #Bergamoisrunning, to reassure clients. It insisted the outbreak was no worse than elsewhere, that the "misleading sensation" of its high number of infections was due to aggressive testing, and that production in steel mills and other industries was unaffected.
Confindustria launched its own campaign in the larger Lombardy region, echoing that message, #Yeswework. Milan's mayor proclaimed that "Milan doesn't stop."

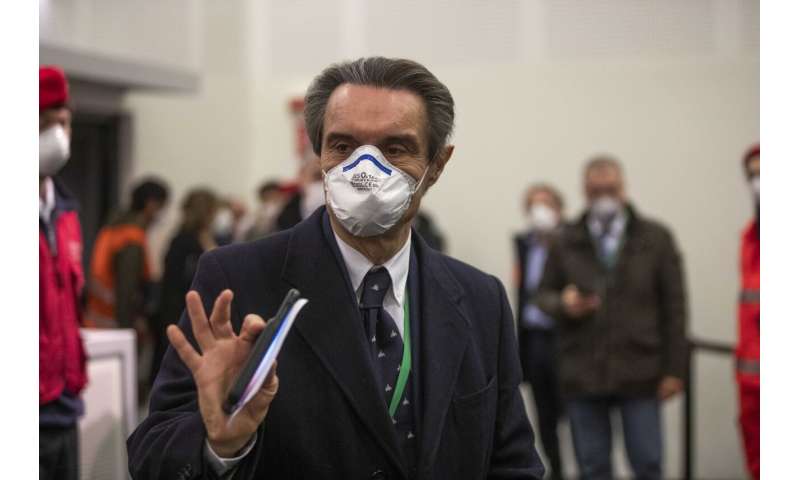
Giulio Gallera, Health Counselor for the Lombardy Region attends a news conference presenting a new hospital Ospedalefieramilano to treat coronavirus patients in Milan, Italy, Tuesday, March 31, 2020. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. The intensive care hospital was unveiled to great fanfare on March 31, the fruit of a 21 million euro fundraising campaign spearheaded by Lombardy's Fontana, of the right-wing League party, to try to relieve pressure on the region's overtaxed ICUs which on that date were near capacity at 1,324 patients. In the end, the Milan field hospital was barely used, treating only a few dozen patients. (AP Photo/Luca Bruno)
At the time, Confindustria Lombardy chief Marco Bonometti acknowledged the "drastic measures" needed in Lodi but sought to lower the sense of alarm.
"We have to let people know they can go back to life as it was, while safeguarding their health," he said.
Even after the Rome-based national government locked down all of Lombardy March 7, it allowed factories to stay open, sparking strikes from workers worried their health was being sacrificed to keep Italy's industrial engine rolling.
"It was a huge error. They should have taken the example where the first cluster was found," said Giambattista Morali of the metalworkers' union in the Bergamo town of Dalmine. "Keeping factories open didn't help the situation; obviously it worsened it."
Eventually, all but essential production was shut down nationwide March 26. Confindustria's national president, Carlo Bonomi, has been urging that industry be reopened, but in a safe way.
"The paradigm has changed," Bonomi told RAI state television. "We can't make Italians secure if we don't reopen factories. But how do we make factories safe to secure Italians?"
It's a tough sell, given Lombardy is still adding an average of 950 infections daily, while other regions add from a few dozen to 500 apiece, with most new cases registered in nursing homes. Italy is set to begin a gradual reopening May 4, leading with regions farther south where the outbreak is more under control.

In this Tuesday, March 17, 2020 file photo, a woman walks outside the Pesenti Fenaroli hospital, in Alzano Lombardo, near Bergamo, the heart of the hardest-hit province in Italy's hardest-hit region of Lombardy, Italy. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. Two days after Italy registered its first positive case in the Lombard town of Codogno, sparking a lockdown of Codogno and nine nearby towns, another positive case was registered Feb. 23 more than an hour's drive away in the hospital of Alzano Lombardo in the province of Bergamo. Whereas the emergency room of Codogno's hospital was shuttered after its first positive case, the ER of Alzano's hospital reopened after a few hours of cleaning, fast becoming one of Bergamo's main sources of contagion. (AP Photo/Luca Bruno, File)
Lombardy probably will be last to fully open, with its 72,000 confirmed cases, 70% of Italy's total, and estimates that the real number could be 10 times that.
A COSTLY FIELD HOSPITAL
Perhaps no initiative better illustrates Italy's confused coronavirus response than the 200-bed field hospital built in less than two weeks on the grounds of Milan's convention center.
The hospital was unveiled to great fanfare on March 31, the fruit of a 21 million euro ($23 million) fundraising campaign headed by Lombardy's governor, a member of the right-wing League party, to try to ease pressure on regional ICUs, which on that date were near capacity at 1,324 patients.
The national civil protection agency opposed the plan, arguing it could never equip it with ventilators or personnel in time. Instead, the agency, which reports to the rival 5-Star-Democratic government in Rome, preferred smaller field units set up outside hospitals and a program to move critical patients elsewhere.
In the end, the Milan field hospital was barely used, treating only a few dozen patients. Since it opened, Lombardy has seen pressure on its ICUs fall considerably, with just over 700 people needing intensive care today.
Fontana, the governor, defended the decision and said he would do it again, telling Radio 24: "We had to ... prepare a dam in case the epidemic overcame the embankment."
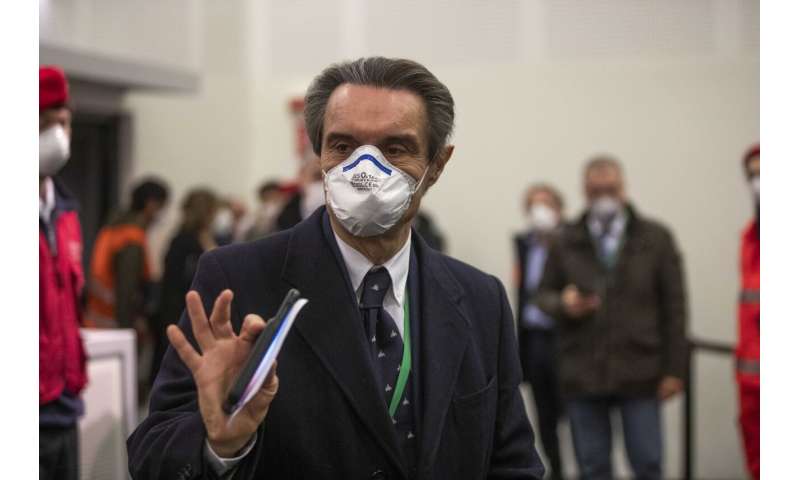
Lombardy region president Attilio Fontana arrives to attend a news conference presenting a new hospital Ospedalefieramilano to treat coronavirus patients in Milan, Italy, Tuesday, March 31, 2020. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. The intensive care hospital was unveiled to great fanfare on March 31, the fruit of a 21 million euro fundraising campaign spearheaded by Lombardy's Fontana, of the right-wing League party, to try to relieve pressure on the region's overtaxed ICUs which on that date were near capacity at 1,324 patients. In the end, the Milan field hospital was barely used, treating only a few dozen patients. (AP Photo/Luca Bruno)
NURSING HOME 'MASSACRE'
While the regional government was focused on building the field hospital and scrambling to find ICU beds, its testing capacity lagged and Lombardy's nursing homes were in many ways left to fend for themselves.
Hundreds of elderly have died in Lombardy and across Italy in what one WHO official has termed a "massacre" of those most vulnerable to the virus. Prosecutors are investigating dozens of nursing homes, as well as measures taken by local health authorities and the regional governments that may have worsened the problem.
Lombardy has more nursing homes than any other region, housing at least 24,000 elderly, and it registered more dead at those facilities than others too. Of the 3,045 dead from Feb. 1 to April 15 in the region, 1,625 were either positive for the virus or showed its symptoms, according to preliminary results from a survey by the Superior Institute of Health.
Of particular attention to prosecutors was the March 8 decision by the regional government to allow recovering COVID-19 patients to be put in nursing homes to free up hospital beds. The region says it required the homes guarantee the patients would be isolated, but it's not clear who was responsible to ensure that or whether anyone checked.
Even before that, staff at some homes said management prevented them from wearing masks for fear of scaring residents.
A March 30 regional decree, again aimed at easing pressure on Lombardy's ICUs, told nursing home directors to not hospitalize sick residents over 75 if they had other health problems. The decree said it was "opportune to treat them in the same facility to avoid further risks of decline in transport or during the wait in the emergency room."

In this Tuesday, March 17, 2020 filer, death notices are seen on a board along an empty road in Alzano Lombardo, near Bergamo, the heart of the hardest-hit province in Italy's hardest-hit region of Lombardy, Italy, Tuesday, March 17, 2020. As Italy prepares to emerge from the West's first and most extensive coronavirus lockdown, it is increasingly becoming apparent that something went terribly wrong in Lombardy, the hardest-hit region in Europe's hardest-hit country. Two days after Italy registered its first positive case in the Lombard town of Codogno, sparking a lockdown of Codogno and nine nearby towns, another positive case was registered Feb. 23 more than an hour's drive away in the hospital of Alzano Lombardo in the province of Bergamo. Whereas the emergency room of Codogno's hospital was shuttered after its first positive case, the ER of Alzano's hospital reopened after a few hours of cleaning, fast becoming one of Bergamo's main sources of contagion. (AP Photo/Luca Bruno, File)
For the elderly at a nursing home in Nembro, one of the hardest-hit towns in Bergamo province, the decree amounted to a death warrant. But it wasn't the first or only one that gave the home's managers the sense that they were being abandoned.
When management proactively barred visitors on Feb. 24 to try to protect residents and staff from infection, local health authorities responded by threatening sanctions and a loss of accreditation for cutting off family visits, said the facility's new director, Valerio Poloni.
In the end, 37 of the 87 residents died in February and March. Its doctor, as well as Poloni's predecessor as director, also tested positive, were hospitalized and died. A nursing home resident couldn't get admitted to the hospital in late February because the ER was too crowded.
The facility's health director, Barbara Codalli, said she was told to use her existing resources to treat the sick. "The patient returned a few hours later, and a few days later the patient died," she told La7 television.
To date, none of the surviving residents has been tested. Poloni said tests were expected to begin in a few days. Two more residents died so far in April, but the situation seems under control.
''We are tranquil,'' he said.
© 2020 The Associated Press. All rights reserved..
Colleen Barry in Soave, Italy, contributed to this report.
Italy's far-right League hurt by response to coronavirus in heartland
Sara Rossi, Emilio Parodi APRIL 25, 2020
MILAN (Reuters) - The coronavirus crisis has left Italy’s northern economic powerhouse a disaster zone and raised awkward questions for far-right opposition leader Matteo Salvini’s League party, which has dominated the region’s politics for years.
Ever since its creation as a separatist movement in the 1980s, the League’s heartland has been in the prosperous small towns of Lombardy around the financial capital Milan, the area that has now borne the brunt of the COVID-19 crisis.
Under Salvini’s leadership, the League has become Italy’s strongest party, mixing nativist and anti-immigration policies with harsh criticism of the European Union that has at times included threats to quit the euro.
But the crisis in his home region has dented Salvini’s once all-conquering image, making it harder to land attacks on Prime Minister Giuseppe Conte’s coalition government in Rome, which Salvini quit spectacularly last year in a failed attempt to force a new election.
Two months after the first outbreak of COVID-19 in a small town outside Milan, Lombardy remains one of the world’s worst-hit regions, accounting for half of Italy’s 26,000 dead.
As local families have seen elderly relatives dying alone in overflowing hospitals or nursing homes, the League-led regional government, which runs the health system, has faced increasing criticism from its own supporters.
“For us seeing the hospitals full and the ambulances that didn’t arrive was unthinkable,” said Ivan Dallagrassa, who runs a building company in Gorno near Bergamo and lost an uncle and probably an aunt to COVID-19. “At the last elections I voted for the League because I liked Salvini but I wouldn’t do it again.”
The troubles in Lombardy have started to undermine national support for the party, which had already been losing ground to parties like the right-wing Brothers of Italy group, while Conte has enjoyed sky-high approval ratings of over 60 percent.
A poll on Sunday by the Ipsos institute for the Corriere della Sera newspaper put the League on 25.4 percent, down from 31.1 a month ago, accelerating a steady slide since it took 34.3 to become the largest party in European elections a year ago.
HALF OF ITALY’S DEAD
The regional government has been criticised for communication missteps, policy zig-zags, lack of early testing and failing to procure enough protective equipment. Magistrates have begun investigating a wave of deaths in the region’s nursing homes.
Salvini’s own position, like those of many politicians on all sides, has shifted during the crisis. Early on he blamed foreigners, demanding to close Italy’s borders; he was then a sceptic of shutting down business, before ultimately joining calls for a strict lockdown.
Whatever stance he has taken on the national level, his fortunes are tied to the performance of his party in administering the region it dominates.
Local officials point to actions they have taken, including setting up a huge emergency hospital, bringing in millions of protective masks and setting aside billions of euros to boost the economy.
“There’s no justification for these attacks,” regional governor Attilio Fontana, a close Salvini ally, told local TV station ETV last week, saying much of the criticism was motivated by “political speculation”.
But while criticism from opponents may be predictable, many normally sympathetic voices have also expressed deep misgivings.
“The main criticism I would make of the management of this crisis by the region of Lombardy is organisational failure,” said Roberto Francese, who heads a centre-right administration as mayor of Robbio, 50 kilometres southwest of Milan.
Lombardy officials have also had to defend pre-crisis health reforms, which favoured big hospitals and private sector providers and stripped down local services now seen as vital to treating patients before they end up in intensive care.
“Local medical services have gone backwards, it’s true,” said Lorenzo Demartini, a hospital radiologist and a former League mayor of Mede, near Milan. “They have been dismantled, I can confirm it.”
By contrast, the League governor in neighbouring Veneto, Luca Zaia, has emerged strengthened from the crisis, widely praised for decisive action backed by a strong local health system that kept hospital admissions down.
While the League has weathered previous storms, Lorenzo Pregliasco, head of political analysis firm Youtrend, said the “mishandling of a huge crisis affecting ordinary people” was a very different problem from the financial scandals that regularly blight Italian politics.
“The party’s appeal is based on Salvini’s charismatic leadership but also on a reputation for pragmatic and effective government at local level,” he said. “That has been damaged.”