Manitoba woman devastated over delay in MAID for mental illness
medical assistance in dying (MAID)
CBC
Sun, February 4, 2024

Cathy Van Buskirk says she is heartbroken by the federal government's delay on medical assistance in dying because of mental illness. (Submitted by Cathy Van Buskirk - image credit)
Cathy Van Buskirk, who lives with complex and debilitating mental disorders, says she is heartbroken by the federal government's decision to delay her ability to access a medically assisted death.
Eligibility for medical assistance in dying (MAID) was set to expand in March to include people with mental illness, something that had given Van Buskirk hope that her suffering from severe mental illness would come to a peaceful end on her terms.
But federal Health Minister Mark Holland introduced legislation Thursday that would delay the expansion of MAID to include those suffering solely from mental illness until 2027, a move he said was needed until Canada's health-care system is ready to implement the expansion.
Van Buskirk says the delay is exclusionary and stigmatizes an already vulnerable population.
"The government's making it even worse by not recognizing and not including us," she said. "My illness causes me grievous amounts of pain and suffering, just as someone who would suffer a physical one."
The 56-year-old Brandon resident says all treatments she has tried over several years have failed to end the suffering created by body dysmorphia, OCD, depression and anxiety. Van Buskirk says MAID would allow her to die on her terms and end the pain she lives with every day.
Holland says the decision to delay the expansion until after the next federal election has nothing to do with electoral politics, but was made to ensure the health-care system is ready and people are properly trained.
This comes after recommendations from a parliamentary committee warning Canada's health system is not ready to allow MAID for people with only a mental illness because there's too much work to do before the legislation is set to expand.
Medical accessibility
Van Buskirk says she has had tremendous health care to support her mental disorders. For 20 years medications helped her. But she says treatments stopped working for her five years ago.
She has had 12 shock treatments, 12 ketamine infusions, cognitive behaviour therapy, numerous counselling sessions, exposure therapy, a week in a psychiatric ward and other treatments to try to treat her mental disorders.
"Your brain is a part of your anatomy, and it's my brain that's sick," Van Buskirk said, adding her brain doesn't make serotonin anymore — the chemical that people need to feel happy.
She says she now finds it hard to leave the house and no longer enjoys the things she once loved like reading, gardening, travelling and praying.
Van Buskirk says she has attempted suicide three times, traumatizing both her and her family.
"I feel … profound sense of loss and sadness every day of my life. Nothing brings me joy or happiness or peace," she said.
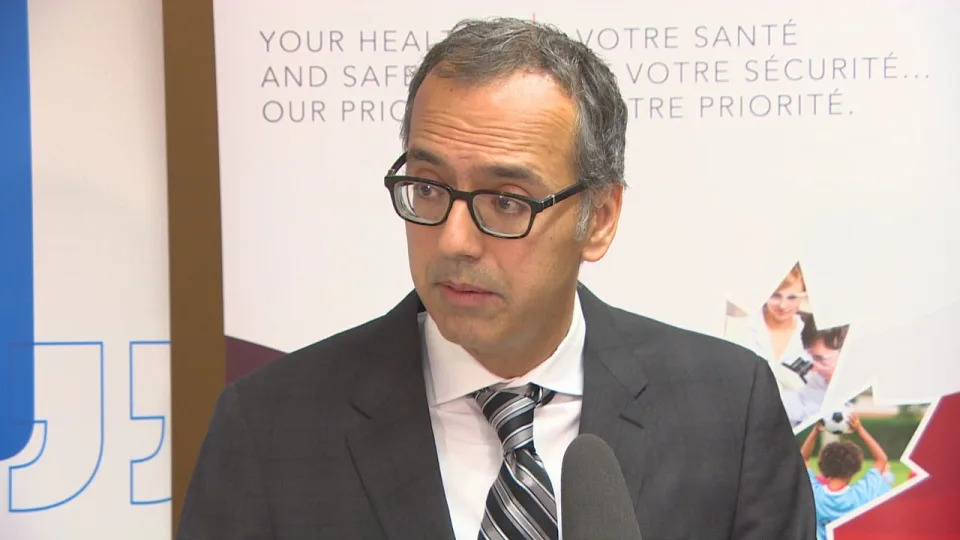
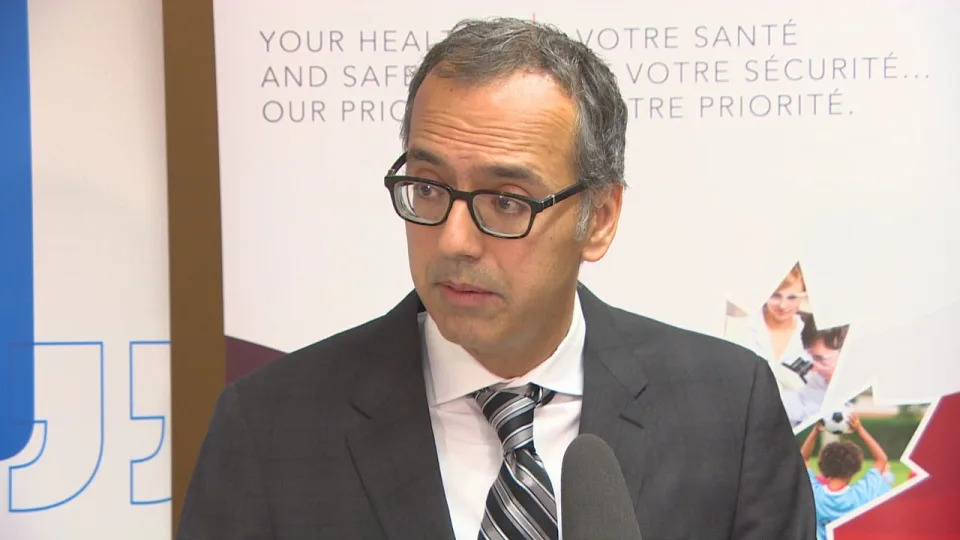
Dr. Jitender Sareen, medical director of the Winnipeg Regional Health Authority mental health program, says new treatment beds and mobile clinical support services are an important step in dealing with the growing meth problem in the city. Dr. Jitender Sareen, medical director of the Winnipeg Regional Health Authority mental health program, says MAID for mental illness needs to be deferred indefinitely. (Megan Goddard/Radio-Canada)
Dr. Jitender Sareen, head of the University of Manitoba's psychiatry department and medical director of the Winnipeg Regional Health Authority's mental health program, says in his field there is a lot of concern about the expansion of MAID.
He was one of the psychiatry chairs to call for an indefinite pause for MAID for mental illness because there is no scientific evidence to help guide MAID decisions when it comes to mental health and addictions. He says this also affects how potential safeguards could be put in place.
"It becomes a challenge to say … especially for mental illness, who's going to get better and who's not," Sareen said.
He said that has been the challenge with this legislation — setting an arbitrary deadline for a procedure for someone who's not dying — because it still requires more evidence and assurances that it's safe.
Sareen expects it will take more than three years for the appropriate clinical standards to be in place.
"The distress of the majority of psychiatrists and mental-health professionals in this area is to say the person wants MAID [but] doesn't mean that they should have access to MAID because they want it," he said.
What's needed in Canada, Sareen says, is greater investment in mental health and addiction services. He compares it to a new cancer drug — mental health treatments should be available to anyone who needs it.
"There is such an inequity in access to mental health addiction services, especially for our rural and First Nations communities, and this disparity would get even worse," he said. "We have not been spending enough energy and time on helping, having these cross-provincial, federal, community dialogues on how do we make psychotherapy available, how do we make equitable access to addictions care."
A Shared Health Spokesperson says when MAID came into effect in June 2016, the province saw 36 written requests for the service and 24 deaths. In 2023, that number had grown to 366 requests and 236 deaths.
The spokesperson noted there are more MAID approvals each year than MAID deaths — mainly due to voluntarily withdrawn requests or individuals dying before receiving MAID.
Health Canada reported 13,241 people received medically assisted deaths in 2022 — a 31.2 per cent jump over 2021.
It said 44,958 people have received medically assisted deaths since the introduction of federal legislation in 2016.
Broader mental health strategy needed
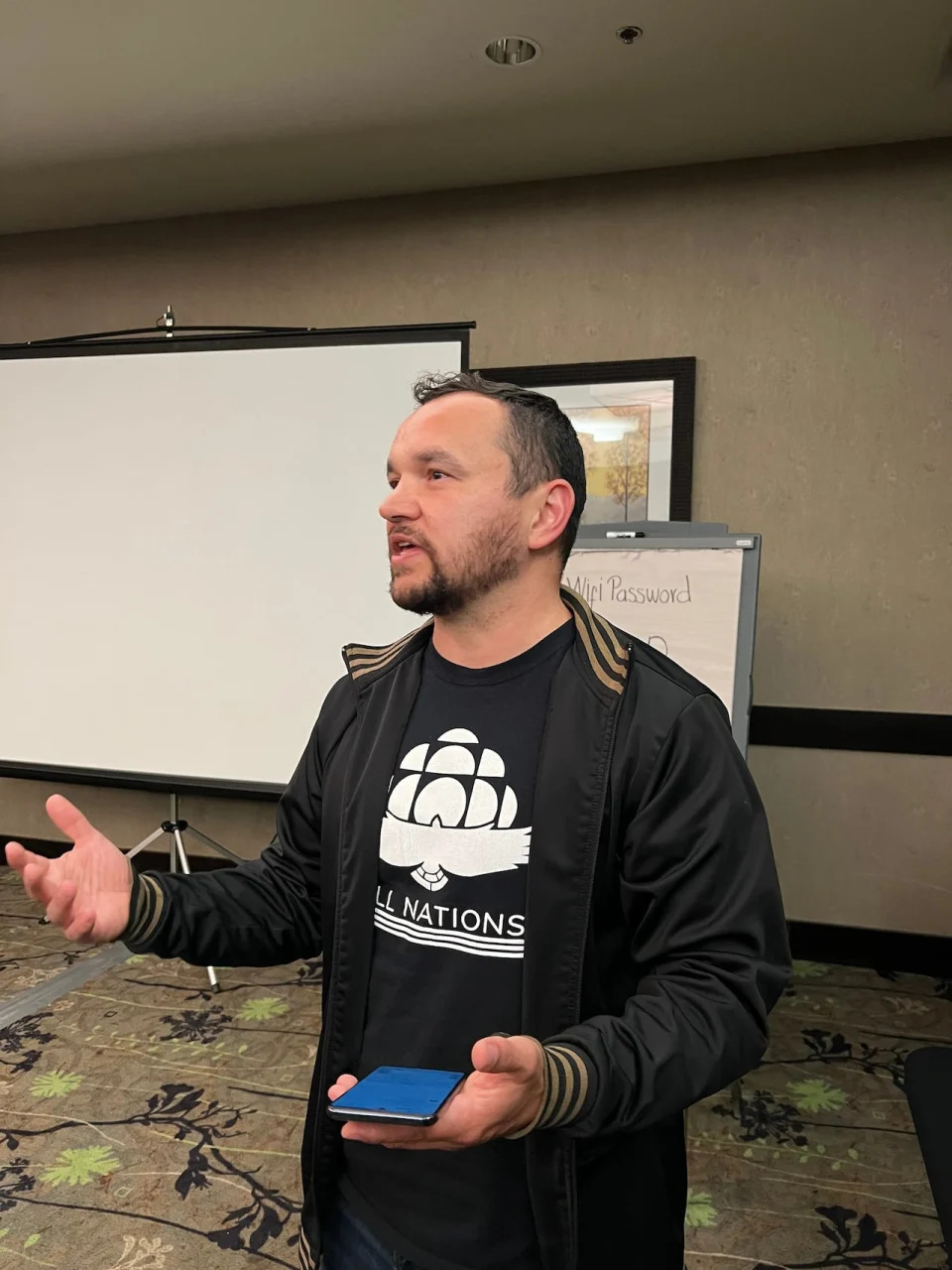
Neil McArthur, director of the Centre for Professional and Applied Ethics at the University of Manitoba said while MAID could be a tool in easing suffering, it should be part just one part of a broader discussion and strategy around how people with mental illness are treated.
McArthur says the situation is difficult to balance from an ethical standpoint. He says people have a right to bodily autonomy, and how they live their lives — therefore they have a right to decide how to end their lives.
But he says mental illness can affect someone's autonomy — the capacity to make an informed, uncoerced decision.
"That's not to say people with mental illness lose their capacity for decision making," said McArthur.
"But it does affect how they view the future and how they view their lives."

Neil McArthur, director of the Centre for Applied Ethics at the University of Manitoba, says Manitoba Liquor & Lotteries is not fulfilling its moral and legal responsibilities.
Neil McArthur, director of the Centre for Applied Ethics at the University of Manitoba, says MAID needs to be part of a broader mental health strategy in Canada. (Tyson Koschik/CBC)
He said MAID for people with mental illness shouldn't be seen as an "easy way out," or a "cheaper way out" for society.
"It absolutely needs to be part of a broader system where we care for people with mental health issues and we are not doing that right now. We are failing right now," he said.
"I personally do believe that people should in cases of grievous mental suffering have access to MAID. But it cannot happen until we have a better system for supporting them and helping them get better."
He said clear rules are needed on who qualifies for MAID, and who gets to say who qualifies for MAID — and he understands why people are frustrated by the "endless delays" in producing a comprehensive mental health strategy.
"They have to make progress on this. They can't keep pushing this and pushing this and pushing this and saying well we need safeguards, well we need safeguards. Well you've had years now," he said.
Van Buskirk says she has worked with many health-care professionals to address her mental disorders, and has gone through several screening processes in her choice to pursue MAID.
She does not want to put her family through the trauma of her death by suicide, but now she feels like she's out of options.
"The pain and the suffering that we go through is … just as debilitating as physical pain," Van Buskirk said. "I could die at peace with my family by my side … just like any other Canadian who has a serious illness."