CBC
Fri, April 19, 2024
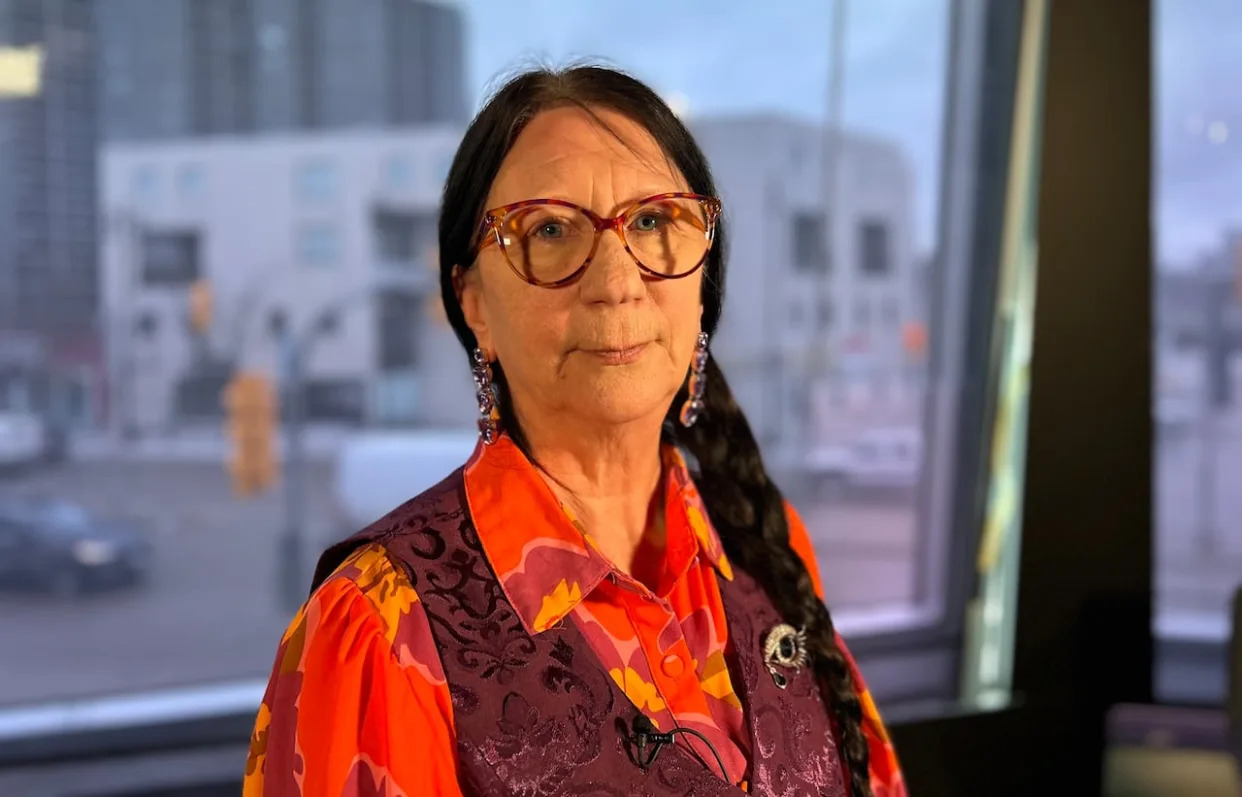
Arlene Last-Kolb says the solution to dealing with the crisis of drug overdose deaths is to ensure a safe supply of drugs for people struggling with addiction while they seek help. (Kevin Nepitabo/CBC - image credit)
A safe place to consume drugs is vital to saving lives, but even more crucial in the harm-reduction approach is providing a safe supply of drugs, says a Winnipeg mom whose son died from fentanyl poisoning.
"We won't change things enough unless we do something about the supply. That's the most important thing that we have to move forward on," said Arlene Last-Kolb, co-founder of Overdose Awareness Manitoba and member of Moms Stop the Harm.
"We just have to convince the people that it can really make the difference, that this is the right way to go. We need to do this today."
Since the death of her 24-year-old son Jessie in July 2014, Last-Kolb has lobbied for compassionate treatment, including a safer drug supply.
Street drugs are now being laced with highly addictive opioids and other substances like animal tranquilizers, making them extremely dangerous, in many cases.
Last year, preliminary data says there were 445 suspected overdose deaths in Manitoba, with 54 in December alone. The province says there were 132 drug-related deaths the year Jessie died, 96 of which were ruled accidents.
"I want everybody to know that we're not just talking about people that live on the street. People are dying in our homes, in our basements," said Last-Kolb.
You can't keep telling people to not take drugs if they are hooked — it's not possible for them, she added.
Stigma and shame also keep them from seeking help and push them to dangerous places to feed the addiction, said Last-Kolb.
The solution, she said, is to give them what they need to stay alive while they seek help.
"Our government has the power to change things. Replace the toxic street drugs with a regulated supply of drugs. We could look at it the same way that we've done cannabis, that we've done alcohol," she said.
"Let's not call it safe supply [or] safe regulated supply. Let's call it doing the right thing."
By starting with a safe supply and an open discussion, it may be possible for someone to get the support they need to work toward easing off opioids, said Last-Kolb.
"We can't keep letting fentanyl win. Jessie sure didn't want to die."
Report calls for 'safe and sanctioned drug supply'
An independent report released on Thursday, evaluating the first year of Winnipeg's mobile overdose prevention site (MOPS), says while the program has exceeded expectations and prevented many drug deaths, more needs to be done to ensure a safe supply of drugs.
The mobile site, a converted RV operated by Sunshine House, travels around Winnipeg's core area providing a supervised consumption site, while also distributing harm reduction supplies and testing drugs.
In its first year, from October 2022 to October 2023, the MOPS team recorded 26,154 visits, with drugs consumed 7,086 times. There were zero deaths.

Sunshine House's MOPS, or mobile overdose prevention site, travels around Winnipeg's core area providing a safe consumption site while also distributing harm reduction supplies.
Sunshine House's MOPS, or mobile overdose prevention site, travels around Winnipeg's core area providing a safe consumption site while also distributing harm reduction supplies. (Radio-Canada)
The report advocates for the creation of several supervised consumption sites in Winnipeg to increase those benefits.
But "if we truly want to stop toxic drug poisonings, we should look at having a safe and sanctioned drug supply," the report states.
Bernadette Smith, minister of housing, addictions and homelessness, said in a statement Friday the province values advocates' calls for solutions to the drug toxicity crisis, but that it's "not looking at safe supply."
"Our primary focus now is on creating the province's first supervised consumption site and making drug testing available," the minister said. "We will continue to work with community organizations and experts on a harm reduction approach."
The report acknowledges that's an "often politically contentious" subject, but says it "is also a useful tool to reduce the harms caused by toxic drugs and unknown poly-drug combinations."
According to the report, government of Canada early research findings suggest safe supply is associated with a range of benefits, including lower overdose rates, reduced hospital admissions and ER visits, decreased criminal activity, and improved connections to care and treatment for people who have not had those supports.
Last-Kolb said toxic drugs are not only "killing our loved ones every day, but the toxicity is causing such great damage to our loved ones that it is having a rippling effect on our whole community."
"Everybody needs to worry about it because everybody is affected by what is happening in our province, whether that is through death, crime, mental health, everything."
A combination of supervised consumption sites and safer supply would be powerful, but still not enough against the drug crisis, the report states.
"Each of these services are intended to complement a much more robust and holistic range of supports" backed by mental health and crisis response services, holistic housing, and community connections, it says.
"People who use drugs may seek treatment and then relapse many times, and the services must remain available throughout each person's journey."

Although the report bears good news of the efficacy of MOPS, Sunshine House executive director Levi Foy says the mobile site is a 'highly imperfect model' that is not sustainable, adding that a permanent safe consumption site is needed.
Sunshine House executive director Levi Foy says the mobile site is needed but is not the solution, rather it is part of a larger network of care. (Jaison Empson/CBC)
Sunshine House executive director Levi Foy agreed.
"This [MOPS] is part of a larger network, a larger part of caring for one another and caring for individuals in new and unique ways that our current system just is not managing," he said at a news conference on Thursday, where the report was released.
Last-Kolb said she won't stop pushing until that full vision of care is complete.
"I would not be here if I didn't think that this was important," she said. "I will not get my son back. But at least I will know that I did all I could to do the right thing.
"If your child dies, no amount of treatment, no amount of justice, no amount of policing is going to bring them back."
CBC
Sat, April 20, 2024

Premier David Eby said he shares concerns over public safety that have arisen from the province's drug decriminalzation pilot. (Justine Boulin/CBC - image credit)
Scrutiny of B.C.'s drug decriminalization pilot is growing, with public safety concerns that have put the spotlight squarely on the governing NDP as the province moves toward a fall election.
Earlier this week, Vancouver Police Deputy Chief Fiona Wilson testified at a House of Commons health committee hearing about how the pilot is limiting police response to problematic public drug use, including inside hospitals and at bus stops.
"In the wake of decriminalization, there are many of those locations where we have absolutely no authority to address that problematic drug use, because the person appears to be in possession of less than 2.5 grams," Wilson said. "So if you have someone who is with their family at the beach, and there's a person next to them smoking crack cocaine, it's not a police matter."
The decriminalization pilot was introduced in January 2023 and allows adult drug users in B.C. to carry up to 2.5 grams of opioids, cocaine, methamphetamine and ecstasy for personal use without facing criminal charges. Relying on an exemption granted by Health Canada under the Controlled Drugs and Substances Act, it also allows for open drug use in some public spaces.
The province did try to bring in legislation in October to limit public drug use, but it was blocked by the courts.
Premier David Eby said he shares the concerns over public safety and intends to address the issue.
"Simply because we have compassion and concern about those struggling with addiction, does not mean that we need to give up our public spaces, does not mean that we have to have parks and playgrounds that are less safe," said Eby.
The province's options include ending the program, or possibly asking the federal government to bring in more changes to the pilot.

Deputy Chief Constable Fiona Wilson is pictured during an update about a sexual assault cold case where the VPD charged Arturo Garcia Gorjon with four counts of sexual assault, related to crimes that occurred between July 1, 2009 and December 24, 2010 Vancouver, British Columbia on Wednesday, August 30, 2023.
VPD Deputy Chief Constable Fiona Wilson told a parliamentary committe on health the limit on police powers to address the public consumption of illicit drugs is affecting public safety. (Ben Nelms/CBC)
A meeting between Jennifer Whiteside, B.C.'s minister of mental health and addictions, and her federal counterpart Ya'ara Saks is scheduled for next week.
In a statement echoing Eby, Whiteside defended decriminalization as a way to destigmatize addiction and treat it as a healthcare issue instead of a criminal one.
"We maintain that having compassion for individuals struggling with addiction does not preclude the need to ensure the safety of workers and members of the public," said Whiteside.
B.C.'s official opposition has been highlighting illicit drug use in hospitals and the lack of guard rails around the decriminalization pilot.
"We knew it would result in exactly what's happening right now, which is an explosion of drug use taking place in SkyTrains, in restaurants and public spaces," said B.C. United leader Kevin Falcon. "It's been a horrific failure and the thing that is important to recognize is we're not seeing improved results."
Advocates for harm reduction say the answer is not to scrap the pilot, because it is doing some good.
"Let's get to the table and make this work because I want to tell you this, the other way is [drug users go] into isolation. So if [changes are] to alleviate some public consumption in public spaces, I'm all for that," said Guy Felicella, a harm reduction and recovery expert.
The decriminalization pilot was introduced as a measure to address B.C.'s severe overdose crisis. More than 14,000 people have died of toxic drugs in the province since the crisis was declared a public health emergency in April 2016.